Treatment of Newly Diagnosed Myeloma - Transplant Eligible
Poster Session 1
P-131: Daratumumab (dara) as maintenance therapy after autologous stem cell transplantation (ASCT) in patients with multiple myeloma (MM): Results of a phase 2 study
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Azra Borogovac, MD, MS (she/her/hers)
Assistant Clinical Professor
City of Hope National Comprehensive Cancer Center, United States
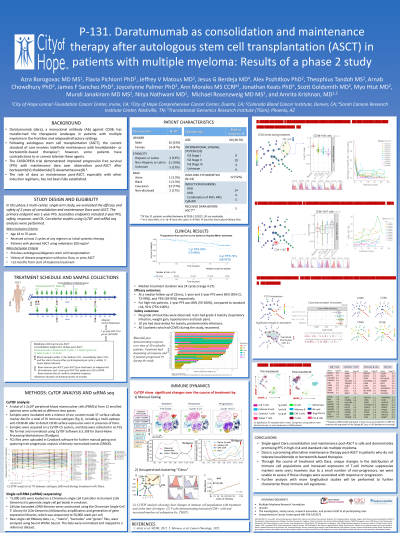
Introduction: The CASSIOPEIA trial demonstrated improved PFS with maintenance dara over observation post-ASCT after bortezomib(V)-thalidomide(T)-dexamethasone(D). The role of dara as maintenance post-ASCT with other induction regimens has not been fully established.
Methods: This open-label single-arm phase 2 study evaluated the safety and efficacy of dara maintenance after upfront high-dose ASCT. Between days 60-120 post-ASCT, pts received iv or sq dara 1800mg weekly (cycles 1-2), biweekly (cycles 3-6), and monthly for a total of 24mos. The primary objective was PFS at 1yr after start of consolidation. Secondary objectives included safety, toxicity, minimal residual disease (MRD), 2yr-PFS and OS.
Results: Of the 31 patients (pts) enrolled between 8/2019-12/2022, 30 are evaluable. Median age was 60 yrs (range 38-70). Eight pts had ISS stage I, 10 had ISS II, 3 had ISS III, 10 pts were unknown. Among the 23 pts with available FISH, 52% had high-risk cytogenetics. Induction regimens included lenalidomide(R)-VD in 14 pts, carfilzomib(K)-RD in 4 pts, and a combination of RVD, KRD and cyclophosphamide-VD in 5 pts. Five pts received dara prior to ASCT. Median treatment duration was 24 cycles (range 4-27) and 19 pts completed 2yrs of therapy. At a median follow-up of 22mos, 1-yr and 2-yr PFS were 85% (95% CI, 73-99%), and 74% (58-92%) respectively. One-yr PFS was 80% (59-100%) and 91% (75%-100%) in the high and standard-risk pts, respectively. During maintenance, 8 pts had a deepening of response. No grade ≥4 toxicities were observed. Four pts had grade 3 toxicity, including respiratory infection, weight gain, hypertension and back pain. Ten pts had dose delays for toxicity, predominantly infections.
CyTOF data from peripheral blood of 12 pts show profound changes in the frequencies of different immune populations including terminally differentiated T cells (TEMRA), activated monocytes, and NK cells. Dara treatment rapidly induced depletion in NK cell populations, which persisted until treatment discontinuation; no association with progression was noted. Four of the 12 pts evaluated progressed within the treatment period ( < 24mos) and had increased CD4 suppressive T cell populations including TIGIT, PD-1, PDL-1 and TIM3-expressing T reg cells and bulk NKT cells. Preliminary scRNA sequencing data in 4 pts showed that upon dara discontinuation, pts had an increase in CD8+ cytotoxic T cell and B regulatory cell populations carrying unique genetic features. Specifically, we found a significant deregulation in the T cell and B cell activation markers including Granulysin, Granzyme A, IFG2R, CXCR4, CXCR5, NFKBID, among others. MRD, scRNA and CyTOF analysis from the rest of the pts will be presented.
Conclusions: Single-agent dara maintenance post-ASCT is safe and demonstrates promising PFS in high-risk and standard-risk MM. In pts progressing on dara, unique changes in the distribution of immune cell populations and increased expression of T cell immune suppressive markers were seen.
Acknowledgments: MMRC
Methods: This open-label single-arm phase 2 study evaluated the safety and efficacy of dara maintenance after upfront high-dose ASCT. Between days 60-120 post-ASCT, pts received iv or sq dara 1800mg weekly (cycles 1-2), biweekly (cycles 3-6), and monthly for a total of 24mos. The primary objective was PFS at 1yr after start of consolidation. Secondary objectives included safety, toxicity, minimal residual disease (MRD), 2yr-PFS and OS.
Results: Of the 31 patients (pts) enrolled between 8/2019-12/2022, 30 are evaluable. Median age was 60 yrs (range 38-70). Eight pts had ISS stage I, 10 had ISS II, 3 had ISS III, 10 pts were unknown. Among the 23 pts with available FISH, 52% had high-risk cytogenetics. Induction regimens included lenalidomide(R)-VD in 14 pts, carfilzomib(K)-RD in 4 pts, and a combination of RVD, KRD and cyclophosphamide-VD in 5 pts. Five pts received dara prior to ASCT. Median treatment duration was 24 cycles (range 4-27) and 19 pts completed 2yrs of therapy. At a median follow-up of 22mos, 1-yr and 2-yr PFS were 85% (95% CI, 73-99%), and 74% (58-92%) respectively. One-yr PFS was 80% (59-100%) and 91% (75%-100%) in the high and standard-risk pts, respectively. During maintenance, 8 pts had a deepening of response. No grade ≥4 toxicities were observed. Four pts had grade 3 toxicity, including respiratory infection, weight gain, hypertension and back pain. Ten pts had dose delays for toxicity, predominantly infections.
CyTOF data from peripheral blood of 12 pts show profound changes in the frequencies of different immune populations including terminally differentiated T cells (TEMRA), activated monocytes, and NK cells. Dara treatment rapidly induced depletion in NK cell populations, which persisted until treatment discontinuation; no association with progression was noted. Four of the 12 pts evaluated progressed within the treatment period ( < 24mos) and had increased CD4 suppressive T cell populations including TIGIT, PD-1, PDL-1 and TIM3-expressing T reg cells and bulk NKT cells. Preliminary scRNA sequencing data in 4 pts showed that upon dara discontinuation, pts had an increase in CD8+ cytotoxic T cell and B regulatory cell populations carrying unique genetic features. Specifically, we found a significant deregulation in the T cell and B cell activation markers including Granulysin, Granzyme A, IFG2R, CXCR4, CXCR5, NFKBID, among others. MRD, scRNA and CyTOF analysis from the rest of the pts will be presented.
Conclusions: Single-agent dara maintenance post-ASCT is safe and demonstrates promising PFS in high-risk and standard-risk MM. In pts progressing on dara, unique changes in the distribution of immune cell populations and increased expression of T cell immune suppressive markers were seen.
Acknowledgments: MMRC
