Treatment of Newly Diagnosed Myeloma - Transplant Eligible
Poster Session 1
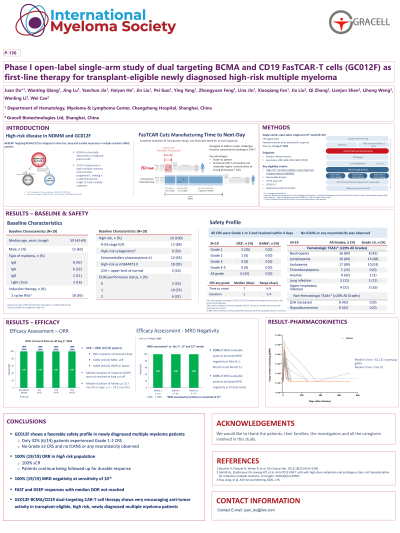
P-136: Phase I open-label single-arm study of dual targeting BCMA and CD19 FasTCAR-T cells (GC012F) as first-line therapy for transplant-eligible newly diagnosed high-risk multiple myeloma
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST
Juan Du
Director
Department of Hematology, Shanghai Changzheng Hospital, United States
Introduction: High-risk (HR) newly-diagnosed multiple myeloma (NDMM) has poor outcomes with standard first-line therapy, even in transplant-eligible (TE) patients (pts). A CAR-T therapy with high efficacy and manageable safety profile would be a potential solution to this significant unmet need. GC012F is an autologous B cell maturation antigen (BCMA) and CD19 dual-targeting CAR-T cells therapy developed on the novel FasTCAR-T enabling next-day manufacturing platform. A single arm, open-label phase I investigator-initiated study (NCT04935580) was conducted in a frontline setting for TE HR NDMM pts to assess the safety and feasibility of GC012F CAR-T cell therapy. Data was presented at ASH 2022 for initial 16 pts. Here we present updated data for study with longer follow-up and 3 additional pts treated (total n=19).
Methods: From June 2022 to April 2023, 19 pts with median age 59 (range 43-69) were treated and evaluated with a single infusion of GC012F at 3 doses levels (DL) of 1E5/kg (n=1), 2E5/kg (n=4), or 3E5/kg (n=14), after a 3-day lymphodepletion consisting of cyclophosphamide and fludarabine. The primary objective of this study was safety; the secondary were pharmacokinetics and efficacy. Cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS) were graded by ASTCT 2019. Efficacy assessment was referred to the IMWG 2016 criteria. Expansion of CAR-T cells and CAR copy numbers were analyzed by flow cytometry and qPCR, respectively.
Results: As of April 12, 2023, the median follow-up time was 14.3 months (range 1.8-21.8 months). All pts had one or more high-risk features including 89% R-ISS stage II or III and 63% with EM. All pts received 2 cycles of induction therapy prior to the infusion. The overall response rate (ORR) was100% and 100% of pts achieved stringent complete response (sCR). All pts achieved minimal residual disease (MRD) negativity assessed by Euroflow with the sensitivity of 10-6. Median duration of response (DOR) and progression-free survival (PFS) were not reached. Only 6 pts (32%) experienced low-grade cytokine release syndrome (CRS), among them 26% was grade 1 (n=5) and 5% grade 2 (n=1). No any grade CRS occurred in other 68% pts. No ICANS or deaths occurred during the study. Robust CAR T-cell expansion was observed in all pts: median Cmax was 62131 (range 8754 - 331159) copies /μg gDNA and the median Tmax was 10 days (range 9-14 days).
Conclusions: Consistent with the previous RRMM cohort treated with GC012F, initial data from this phase I study demonstrated that BCMA-CD19 dual FasTCAR-T GC012F resulted in a deep and durable remission in TE HR NDMM pts with a very favorable safety profile.
These preliminary results emphasize the potential of CAR-T treatment in newly-diagnosed MM pts. Additional studies with larger cohorts and longer follow-ups will further show the significance and benefits of earlier line application of CAR-T therapy for MM pts.
Methods: From June 2022 to April 2023, 19 pts with median age 59 (range 43-69) were treated and evaluated with a single infusion of GC012F at 3 doses levels (DL) of 1E5/kg (n=1), 2E5/kg (n=4), or 3E5/kg (n=14), after a 3-day lymphodepletion consisting of cyclophosphamide and fludarabine. The primary objective of this study was safety; the secondary were pharmacokinetics and efficacy. Cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS) were graded by ASTCT 2019. Efficacy assessment was referred to the IMWG 2016 criteria. Expansion of CAR-T cells and CAR copy numbers were analyzed by flow cytometry and qPCR, respectively.
Results: As of April 12, 2023, the median follow-up time was 14.3 months (range 1.8-21.8 months). All pts had one or more high-risk features including 89% R-ISS stage II or III and 63% with EM. All pts received 2 cycles of induction therapy prior to the infusion. The overall response rate (ORR) was100% and 100% of pts achieved stringent complete response (sCR). All pts achieved minimal residual disease (MRD) negativity assessed by Euroflow with the sensitivity of 10-6. Median duration of response (DOR) and progression-free survival (PFS) were not reached. Only 6 pts (32%) experienced low-grade cytokine release syndrome (CRS), among them 26% was grade 1 (n=5) and 5% grade 2 (n=1). No any grade CRS occurred in other 68% pts. No ICANS or deaths occurred during the study. Robust CAR T-cell expansion was observed in all pts: median Cmax was 62131 (range 8754 - 331159) copies /μg gDNA and the median Tmax was 10 days (range 9-14 days).
Conclusions: Consistent with the previous RRMM cohort treated with GC012F, initial data from this phase I study demonstrated that BCMA-CD19 dual FasTCAR-T GC012F resulted in a deep and durable remission in TE HR NDMM pts with a very favorable safety profile.
These preliminary results emphasize the potential of CAR-T treatment in newly-diagnosed MM pts. Additional studies with larger cohorts and longer follow-ups will further show the significance and benefits of earlier line application of CAR-T therapy for MM pts.
