Treatment of Newly Diagnosed Myeloma - Transplant Eligible
Poster Session 1
P-140: MULTIPLE MYELOMA IN LATIN AMERICA CANCER REGISTRY: THE MYLACRE STUDY
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Vania Hungria, MD, PhD
Associate Professor
Department of Hematology, Clinica São Germano, São Paulo, Brazil
Sao Paulo, United States
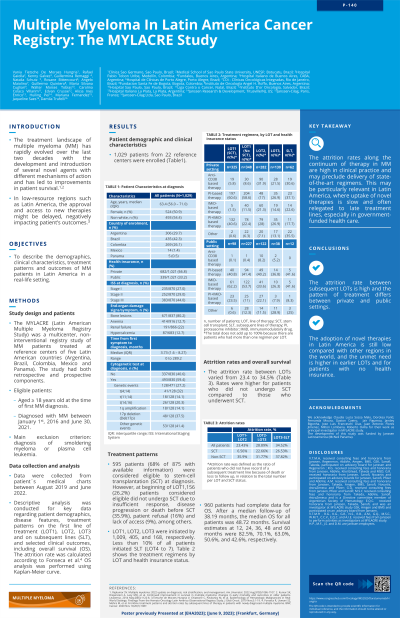
Introduction: The treatment landscape of Multiple Myeloma (MM) has evolved in the last decade with the approval of many innovative drugs, improving patient survival. However, in low-resource regions such as Latin America (LA), the approval and access to novel therapies might be delayed, negatively impacting the outcomes of those patients. The MYLACRE study aimed to describe the MM population demographics and clinical characteristics, and to profile the treatment landscape of LA MM patients.
Methods: This was a retrospective and prospective non-interventional, multicenter study of MM patients from 5 LA countries. Patients aged ≥ 18 diagnosed with MM between January 1, 2016 and June 30, 2021 were included. Data were extracted from medical charts between August 2019 and June 2022 and a descriptive analysis was conducted.
Results: A total of 1,029 patients from 22 reference centers were enrolled, with a median follow-up of 26.8 months. Two thirds (66.8%) had private health insurance coverage. The median age at diagnosis was 64 years and most patients were diagnosed as International Staging System (ISS) stage III (44%). End-organ damage signs and symptoms at diagnosis were reported in most of the patients, with half of them (45.2%) presenting anemia, 12.7% hypercalcemia, 22% renal disfunction and 80.2% bone lesions. Approximately 60% of the patients underwent a cytogenetic test and, of these, one-third (27%) had a cytogenetic abnormality. From the enrolled patients, 1,003 started the first line of therapy (LOT), 405 LOT2, 168 LOT3, 74 LOT4 and 20 LOT5, resulting in an attrition rate of approximately 23-34% from one LOT to the subsequent LOT. Most patients (69.9%) were eligible for stem cell transplant (SCT) upfront, but, of those, 26.8% did not receive it. The main reason was insufficient response, disease progression or death before SCT. Considering patients who underwent SCT, the majority in both private and public settings received a proteasome inhibitor (PI)-based therapy (60.6%, 40.8% respectively) and considering those who did not undergo SCT, the majority in the private setting received a PI-based therapy (58.6%), while in the public setting the majority received an immunomodulatory drug (IMiD) based therapy (53.7%). For LOT2, anti-CD38 based regimens were the most received in the private setting (31.9%) and PI-based regimens for the public setting (40.2%). The median progression-free survival (PFS) of LOT1 was 40 months, LOT2 15.9 months, LOT3 8.9 months, and later LOT 4.6 months. The median overall survival (OS) for all patients was 48.9 months.
Conclusions: The attrition rate between subsequent LOTs is high and the pattern of treatment differs between private and public settings. The adoption of novel therapies in LA is still low compared with other regions in the world, and the unmet need is higher in earlier LOTs and for patients with no health insurance.
Methods: This was a retrospective and prospective non-interventional, multicenter study of MM patients from 5 LA countries. Patients aged ≥ 18 diagnosed with MM between January 1, 2016 and June 30, 2021 were included. Data were extracted from medical charts between August 2019 and June 2022 and a descriptive analysis was conducted.
Results: A total of 1,029 patients from 22 reference centers were enrolled, with a median follow-up of 26.8 months. Two thirds (66.8%) had private health insurance coverage. The median age at diagnosis was 64 years and most patients were diagnosed as International Staging System (ISS) stage III (44%). End-organ damage signs and symptoms at diagnosis were reported in most of the patients, with half of them (45.2%) presenting anemia, 12.7% hypercalcemia, 22% renal disfunction and 80.2% bone lesions. Approximately 60% of the patients underwent a cytogenetic test and, of these, one-third (27%) had a cytogenetic abnormality. From the enrolled patients, 1,003 started the first line of therapy (LOT), 405 LOT2, 168 LOT3, 74 LOT4 and 20 LOT5, resulting in an attrition rate of approximately 23-34% from one LOT to the subsequent LOT. Most patients (69.9%) were eligible for stem cell transplant (SCT) upfront, but, of those, 26.8% did not receive it. The main reason was insufficient response, disease progression or death before SCT. Considering patients who underwent SCT, the majority in both private and public settings received a proteasome inhibitor (PI)-based therapy (60.6%, 40.8% respectively) and considering those who did not undergo SCT, the majority in the private setting received a PI-based therapy (58.6%), while in the public setting the majority received an immunomodulatory drug (IMiD) based therapy (53.7%). For LOT2, anti-CD38 based regimens were the most received in the private setting (31.9%) and PI-based regimens for the public setting (40.2%). The median progression-free survival (PFS) of LOT1 was 40 months, LOT2 15.9 months, LOT3 8.9 months, and later LOT 4.6 months. The median overall survival (OS) for all patients was 48.9 months.
Conclusions: The attrition rate between subsequent LOTs is high and the pattern of treatment differs between private and public settings. The adoption of novel therapies in LA is still low compared with other regions in the world, and the unmet need is higher in earlier LOTs and for patients with no health insurance.
