Cellular and T cell engager Immunotherapy
Poster Session 1
P-019: Novel combination immunotherapy for relapsed/refractory multiple myeloma (RRMM): initial Phase 1 safety run-in results for cevostamab in combination with pomalidomide and dexamethasone
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Tomas Jelinek, MD, PhD
Associate Professor
University Hospital Ostrava and University of Ostrava, Ostrava, Czech Republic, Czech Republic
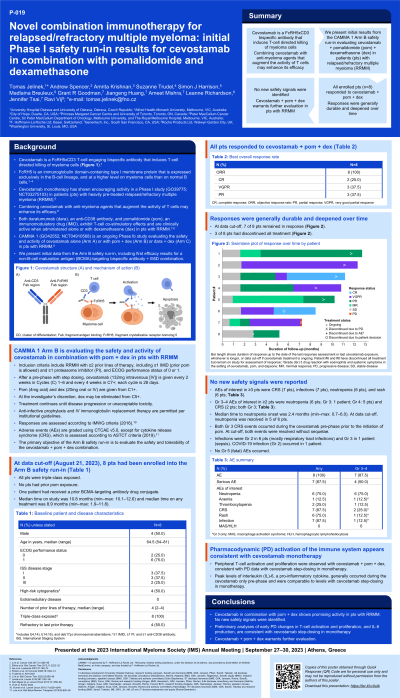
Introduction: Cevostamab, a FcRH5xCD3 bispecific antibody that facilitates T-cell directed killing of myeloma cells, has shown encouraging activity as monotherapy in patients (pts) with heavily pre-treated RRMM in a Phase 1 study (GO39775; NCT03275103; Trudel et al. ASH 2021). Combining cevostamab with anti-myeloma agents that augment the activity of T cells may enhance efficacy (Li et al. Mol Cancer Ther 2023). Both daratumumab (dara), an anti-CD38 antibody, and pomalidomide (pom), an immunomodulatory drug (IMiD), exhibit T-cell co-stimulatory effects and are clinically active when administered alone or with dexamethasone (dex) in pts with RRMM (Lonial et al. Lancet 2016; San Miguel et al. Lancet Oncol 2013). CAMMA 1 (GO42552; NCT04910568) is an ongoing Phase 1b study evaluating the safety and activity of cevostamab alone (Arm A) or with pom + dex (Arm B) or dara + dex (Arm C) in pts with RRMM. We present initial data from the Arm B safety run-in, including the first efficacy results for a non-B-cell maturation antigen (BCMA)-targeting bispecific antibody + IMiD combination.
Methods: Eligible pts must have RRMM and have received ≥2 prior lines of therapy, including ≥1 IMiD and ≥1 proteasome inhibitor. Prior pom exposure is allowed. After a pre-phase with step-up dosing, cevostamab is given intravenously every 2 weeks in Cycles (C) 1–6 (28 days per cycle) and every 4 weeks in C7+. From C1+, pom (4 mg PO) is given on Day (D) 1–21 and dex (20 mg) on D1, 8, 15, and 22. At the investigator’s discretion, dex may be eliminated from C5+. Treatment continues until disease progression or unacceptable toxicity.
Results: At data cut-off (February 20, 2023), 8 pts had been enrolled (median age: 64.5 years). Median prior lines of therapy was 4. All pts were triple-class exposed. Median follow-up was 4.8 months. The objective response rate was 100% (8/8 pts), with one patient (12.5%) in complete response, three pts (37.5%) in very good partial response, and 4 pts (50%) in partial response. At cut-off, all responders (8/8 pts) were in response, with responses deepening over time, and 7/8 pts remained on treatment.
Grade (Gr) 3–4 adverse events (AEs) occurred in 7 pts (87.5%) and were most commonly neutropenia (Gr 3: 12.5%; Gr 4: 37.5%). Cytokine release syndrome (CRS) occurred in 7 pts (87.5%), with Gr 3 CRS in 2 pts. Both Gr 3 CRS events occurred during the cevostamab pre-phase prior to the addition of pom and resolved without sequelae. AEs leading to dose modification or interruption occurred in all pts. There were no Gr 5 (fatal) AEs. One patient discontinued study treatment due to a serious AE (Gr 3 drug reaction with eosinophils and systemic symptoms [DRESS]) in the setting of cevostamab, pom, and dapsone exposure.
Conclusions: Cevostamab plus pom and dex shows promising activity in pts with RRMM and warrants further evaluation to optimize the benefit/risk profile. Biomarker and updated clinical data will be presented.
Methods: Eligible pts must have RRMM and have received ≥2 prior lines of therapy, including ≥1 IMiD and ≥1 proteasome inhibitor. Prior pom exposure is allowed. After a pre-phase with step-up dosing, cevostamab is given intravenously every 2 weeks in Cycles (C) 1–6 (28 days per cycle) and every 4 weeks in C7+. From C1+, pom (4 mg PO) is given on Day (D) 1–21 and dex (20 mg) on D1, 8, 15, and 22. At the investigator’s discretion, dex may be eliminated from C5+. Treatment continues until disease progression or unacceptable toxicity.
Results: At data cut-off (February 20, 2023), 8 pts had been enrolled (median age: 64.5 years). Median prior lines of therapy was 4. All pts were triple-class exposed. Median follow-up was 4.8 months. The objective response rate was 100% (8/8 pts), with one patient (12.5%) in complete response, three pts (37.5%) in very good partial response, and 4 pts (50%) in partial response. At cut-off, all responders (8/8 pts) were in response, with responses deepening over time, and 7/8 pts remained on treatment.
Grade (Gr) 3–4 adverse events (AEs) occurred in 7 pts (87.5%) and were most commonly neutropenia (Gr 3: 12.5%; Gr 4: 37.5%). Cytokine release syndrome (CRS) occurred in 7 pts (87.5%), with Gr 3 CRS in 2 pts. Both Gr 3 CRS events occurred during the cevostamab pre-phase prior to the addition of pom and resolved without sequelae. AEs leading to dose modification or interruption occurred in all pts. There were no Gr 5 (fatal) AEs. One patient discontinued study treatment due to a serious AE (Gr 3 drug reaction with eosinophils and systemic symptoms [DRESS]) in the setting of cevostamab, pom, and dapsone exposure.
Conclusions: Cevostamab plus pom and dex shows promising activity in pts with RRMM and warrants further evaluation to optimize the benefit/risk profile. Biomarker and updated clinical data will be presented.
