Plasma Cell Precursor Disorders
Poster Session 1
P-094: CHARACTERISING RISK AND BIOLOGY OF SMOULDERING MYELOMA FOR EARLY DETECTION OF SYMPTOMATIC MYELOMA: DATA FROM THE UK COSMOS STUDY
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Daniel P. Hughes, MBBS
Myeloma research fellow
UCL Cancer Institute
London, United Kingdom
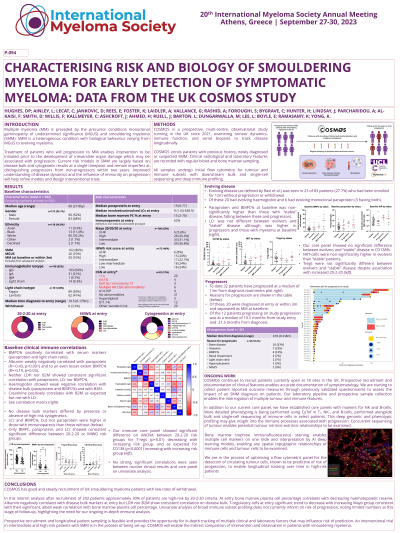
Introduction: Smouldering myeloma(SMM) risk models are largely based on genetics and disease bulk at a single timepoint. Improved understanding of disease dynamics and the influence of immunity on progression will help refine models and design of interventional trials. COSMOS is a prospective multi-centre observational study running in the UK since 2021, examining tumour dynamics, immune function, and serial biopsies to track disease longitudinally.
Methods: COSMOS enrols patients with previous history, newly diagnosed or suspected SMM. Clinical, radiological and laboratory features are recorded with regular blood and bone marrow(BM) sampling. All samples undergo initial flow cytometry for tumour and immune subsets with downstream bulk and single cell sequencing and deep immune profiling.
Results: We recruited 167 patients, median age 69yr (range 27-85), 47.3% male. At entry 82% were SMM, 10.5% MGUS and 7.5% myeloma by CRAB criteria(excluded from subsequent results). Median (range) paraprotein, light chain ratio(LCr) and BM plasma cell percentage(BMPC%) were 18.5g/L(1-77), 8.28(1.04-638.9), and 15(5-60). 43.8% had one or more high-risk cytogenetic lesions. 30%, 28%, 25%, 17% were low, low-intermediate, intermediate, and high-risk(IMWG). 7(4.2%) had ultra high-risk(UHR) disease(SLiM criteria). Median follow-up 10months(range 1-24) with low rate of withdrawal (3.6%).
At entry there was negative correlation between BMPC%/paraprotein and albumin(p=0.02 and p< 0.001). Paraprotein negatively correlated with haemoglobin(p=0.04) and LDH(p=0.04). BMPC% negatively correlated with CD11b+ myeloid cells(p=0.019). CD4/8+ T-cells, Tregs, and NK-cells did not correlate with disease bulk or other immune cell frequencies.
In total 21 patients progressed at median 11m(range 1-130) from diagnosis, 12 within 3 months of study entry and were excluded from our analysis of risk factors based on registration parameters. 12(57%) had bone disease. Of the 9 progressing on study at median 28m(4-130) from diagnosis. 66% were high-risk with paraprotein, LCr, and BMPC% significantly higher than non-progressors. No significantly different alterations in routine biochemical parameters or immune cells by 12m from entry were seen between progressors and non-progressors. 6/7 UHR patients have not progressed.
Our laboratory pipeline includes scRNAseq on BM cells. For one progressing patient, we observed longitudinal clonal expansion of CD8+ T cell TCR clones alongside accumulation of proliferating(MKI67+TYMS+) tumour cells consistent with anti-tumour response.
Conclusions: COSMOS has good and steady recruitment of UK SMM patients. BMPC% at entry correlates with decreasing haematopoietic reserve and decreasing albumin. In SMM, LDH does not appear to correlate with disease bulk. Broad immune cell subsets does not inform on risk or progression, indicating the need for our ongoing in-depth immune analysis. Longitudinal scRNA seq may give insight into immune processes associated with progression.
Methods: COSMOS enrols patients with previous history, newly diagnosed or suspected SMM. Clinical, radiological and laboratory features are recorded with regular blood and bone marrow(BM) sampling. All samples undergo initial flow cytometry for tumour and immune subsets with downstream bulk and single cell sequencing and deep immune profiling.
Results: We recruited 167 patients, median age 69yr (range 27-85), 47.3% male. At entry 82% were SMM, 10.5% MGUS and 7.5% myeloma by CRAB criteria(excluded from subsequent results). Median (range) paraprotein, light chain ratio(LCr) and BM plasma cell percentage(BMPC%) were 18.5g/L(1-77), 8.28(1.04-638.9), and 15(5-60). 43.8% had one or more high-risk cytogenetic lesions. 30%, 28%, 25%, 17% were low, low-intermediate, intermediate, and high-risk(IMWG). 7(4.2%) had ultra high-risk(UHR) disease(SLiM criteria). Median follow-up 10months(range 1-24) with low rate of withdrawal (3.6%).
At entry there was negative correlation between BMPC%/paraprotein and albumin(p=0.02 and p< 0.001). Paraprotein negatively correlated with haemoglobin(p=0.04) and LDH(p=0.04). BMPC% negatively correlated with CD11b+ myeloid cells(p=0.019). CD4/8+ T-cells, Tregs, and NK-cells did not correlate with disease bulk or other immune cell frequencies.
In total 21 patients progressed at median 11m(range 1-130) from diagnosis, 12 within 3 months of study entry and were excluded from our analysis of risk factors based on registration parameters. 12(57%) had bone disease. Of the 9 progressing on study at median 28m(4-130) from diagnosis. 66% were high-risk with paraprotein, LCr, and BMPC% significantly higher than non-progressors. No significantly different alterations in routine biochemical parameters or immune cells by 12m from entry were seen between progressors and non-progressors. 6/7 UHR patients have not progressed.
Our laboratory pipeline includes scRNAseq on BM cells. For one progressing patient, we observed longitudinal clonal expansion of CD8+ T cell TCR clones alongside accumulation of proliferating(MKI67+TYMS+) tumour cells consistent with anti-tumour response.
Conclusions: COSMOS has good and steady recruitment of UK SMM patients. BMPC% at entry correlates with decreasing haematopoietic reserve and decreasing albumin. In SMM, LDH does not appear to correlate with disease bulk. Broad immune cell subsets does not inform on risk or progression, indicating the need for our ongoing in-depth immune analysis. Longitudinal scRNA seq may give insight into immune processes associated with progression.
