Cellular and T cell engager Immunotherapy
Poster Session 1
P-034: Alnuctamab (ALNUC; BMS-986349; CC-93269), a BCMA × CD3 T-cell engager, in patients (pts) with relapsed/refractory multiple myeloma (RRMM): latest results from a phase 1 first-in-human clinical study
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

María-Victoria Mateos, MD, PhD
Professor
University Hospital of Salamanca/IBSAL/CIC/CIBERONC, Salamanca, Spain
Salamanca, Spain
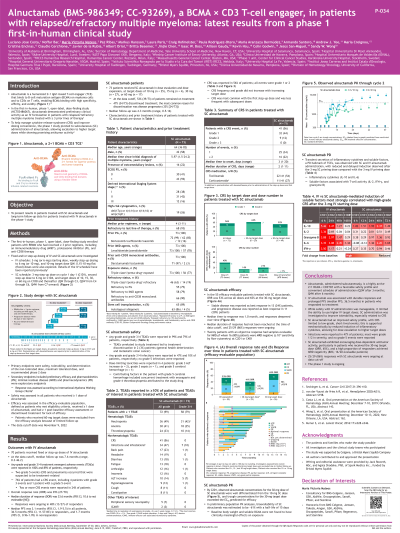
Introduction: ALNUC, a 2+1 T-cell engager (TCE) with bivalent binding to BCMA, demonstrated clinical activity in RRMM in a phase 1 study (NCT03486067). IV ALNUC had a long duration of response (DOR) but resulted in cytokine release syndrome (CRS) in 76% of pts. Subcutaneous (SC) dosing reduced CRS rate and severity, allowing higher target doses with promising antitumor activity. We present long-term data from IV pts and safety and efficacy in SC pts treated in the phase 1 study.
Methods: Pts had ≥3 prior lines of therapy (LOTs), including an immunomodulatory drug, a proteasome inhibitor, and an anti-CD38 therapy. IV ALNUC was given at target doses of 0.15–10 mg with both fixed and step-up dosing (Costa LJ et al. Blood 2019). SC ALNUC was given on D 1, 4, 8, 15, and 22 of cycle 1 (C1), QW in C2–3, Q2W in C4–6, and Q4W in C7+ (28-d cycles). Step-up doses were given on C1D1 (3 mg) and C1D4 (6 mg), and target doses (≥10 mg) on C1D8 and thereafter. Safety and tolerability were primary objectives. Data cutoff was Nov 9 2022.
Results: In total, 70 pts received IV ALNUC. Overall response rate (ORR) was 39% (27/70); median DOR was 33.6 mo (95% CI, 10.6–NA). Median PFS was 3.1 mo (95% CI, 1.9–5.5). CRS was reported in 53 (76%) pts, with grade (G) ≥3 in 5 (7%) pts. Of 73 pts treated with SC ALNUC in dose escalation (target dose: 10 mg, 6; 15 mg, 4; 30 mg, 6; 60 mg, 7) and dose expansion (target dose: 10 mg, 19; 30 mg, 21; 60 mg, 10), median age was 64 y; 42% were female. Pts had a median of 4 prior regimens; 93% were refractory to last LOT, 100%/63% had triple-class exposed/refractory MM; 66%/26% had penta-drug exposed/refractory MM. Median follow-up was 4.3 mo (range, 0.5–16.0); 39 (53%) pts were on treatment at data cutoff. Any-G/G3–4 treatment-emergent adverse events occurred in 99%/79% of SC pts; most common were CRS (56%/0%), neutropenia (49%/42%), infections (47%/10%), anemia (41%/25%), and thrombocytopenia (33%/14%). SC pts had CRS limited to G1 (44%) or G2 (12%); 35 pts received ≥1 concomitant medication for CRS, including tocilizumab (30%) and/or corticosteroids (15%). Median time to CRS was 3 d (range, 1–20); median duration was 2 d (range, 1–11). SC ALNUC bioavailability was ~61%; t½ was 15 d. Trough concentrations at the 30-mg target dose exceeded levels predicted for efficacy by C2D1. In 55 efficacy-evaluable pts receiving SC ALNUC, ORR was 53% across all doses and 65% at the 30-mg target dose; 20/29 responders were minimal residual disease (MRD)-evaluable, of whom 16 (80%) were MRD-negative (10e-5 sensitivity) at C2D1 or C4D1. Median time to response was 1.0 mo (95% CI, 0.7–1.3); 25 responses (86%) were ongoing.
Conclusions: IV ALNUC led to durable responses in heavily pretreated pts with RRMM. SC ALNUC had an improved safety profile vs IV ALNUC, with CRS limited to low-grade, short-lived events. SC ALNUC showed promising dose-dependent antitumor activity and a high proportion of responders were MRD-negative. The phase 1 study is ongoing. Presented at EHA 2023. Wong SW et al. Abstract P883.
Methods: Pts had ≥3 prior lines of therapy (LOTs), including an immunomodulatory drug, a proteasome inhibitor, and an anti-CD38 therapy. IV ALNUC was given at target doses of 0.15–10 mg with both fixed and step-up dosing (Costa LJ et al. Blood 2019). SC ALNUC was given on D 1, 4, 8, 15, and 22 of cycle 1 (C1), QW in C2–3, Q2W in C4–6, and Q4W in C7+ (28-d cycles). Step-up doses were given on C1D1 (3 mg) and C1D4 (6 mg), and target doses (≥10 mg) on C1D8 and thereafter. Safety and tolerability were primary objectives. Data cutoff was Nov 9 2022.
Results: In total, 70 pts received IV ALNUC. Overall response rate (ORR) was 39% (27/70); median DOR was 33.6 mo (95% CI, 10.6–NA). Median PFS was 3.1 mo (95% CI, 1.9–5.5). CRS was reported in 53 (76%) pts, with grade (G) ≥3 in 5 (7%) pts. Of 73 pts treated with SC ALNUC in dose escalation (target dose: 10 mg, 6; 15 mg, 4; 30 mg, 6; 60 mg, 7) and dose expansion (target dose: 10 mg, 19; 30 mg, 21; 60 mg, 10), median age was 64 y; 42% were female. Pts had a median of 4 prior regimens; 93% were refractory to last LOT, 100%/63% had triple-class exposed/refractory MM; 66%/26% had penta-drug exposed/refractory MM. Median follow-up was 4.3 mo (range, 0.5–16.0); 39 (53%) pts were on treatment at data cutoff. Any-G/G3–4 treatment-emergent adverse events occurred in 99%/79% of SC pts; most common were CRS (56%/0%), neutropenia (49%/42%), infections (47%/10%), anemia (41%/25%), and thrombocytopenia (33%/14%). SC pts had CRS limited to G1 (44%) or G2 (12%); 35 pts received ≥1 concomitant medication for CRS, including tocilizumab (30%) and/or corticosteroids (15%). Median time to CRS was 3 d (range, 1–20); median duration was 2 d (range, 1–11). SC ALNUC bioavailability was ~61%; t½ was 15 d. Trough concentrations at the 30-mg target dose exceeded levels predicted for efficacy by C2D1. In 55 efficacy-evaluable pts receiving SC ALNUC, ORR was 53% across all doses and 65% at the 30-mg target dose; 20/29 responders were minimal residual disease (MRD)-evaluable, of whom 16 (80%) were MRD-negative (10e-5 sensitivity) at C2D1 or C4D1. Median time to response was 1.0 mo (95% CI, 0.7–1.3); 25 responses (86%) were ongoing.
Conclusions: IV ALNUC led to durable responses in heavily pretreated pts with RRMM. SC ALNUC had an improved safety profile vs IV ALNUC, with CRS limited to low-grade, short-lived events. SC ALNUC showed promising dose-dependent antitumor activity and a high proportion of responders were MRD-negative. The phase 1 study is ongoing. Presented at EHA 2023. Wong SW et al. Abstract P883.
