Myeloma Microenvironment and immune profiling
Poster Session 3
P-387: Bone marrow immune composition reflects multiple myeloma evolution and influences patients’ outcome
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Anna Maria Corsale (she/her/hers)
PhD student
University of Palermo (Italy)
Palermo, Sicilia, Italy
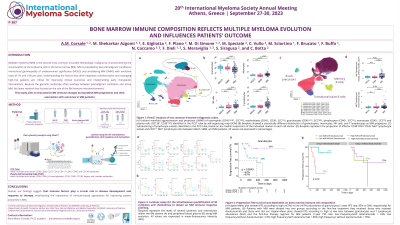
Introduction: Multiple myeloma (MM) is the second most common incurable hematologic malignancy, characterized by the accumulation of clonal plasma cells in the bone marrow (BM). MM is preceded by two premalignant conditions, monoclonal gammopathy of undetermined significance (MGUS) and smoldering MM (SMM), with respective evolution rates of 1% and 10% per year. Understanding the factors that drive neoplastic transformation and managing high-risk patients are critical for improving clinical outcomes and implementing early therapeutic interventions. Because the genomic landscape often overlaps between premalignant conditions and active MM, the latest research has focused on the role of the BM immune microenvironment. This study aims to characterize BM immune changes during MGUS-MM progression and their association with outcome in MM patients.
Methods: We used FlowCT, a semi-automated pipeline for flow cytometry data analysis, to compare the immune composition in the BM of 12 MGUS, 12 SMM, and 63 MM patients stained with two common 8-markers diagnostic tubes. Next, we performed Luminex assays for the simultaneous quantification of 48 cytokines and chemokines using plasma samples of BM and peripheral blood (HD=4, MGUS=12, SMM=12, and MM=12) to obtain a MM immune response profiling.
Results: Progression to clinical MM was associated with a decrease in granulocytes (mean, 74.18% MGUS vs 73.86% SMM vs 65.59% MM; p< 0.05) and an increase in monocytes (mean, 4.97% MGUS vs 4.62% SMM vs 6.77% MM; p< 0.01), T lymphocytes (mean, 6.29% MGUS vs 7.56% SMM vs 11% MM; p< 0.01), and NK cells (mean, 0.88% MGUS vs 1.51% SMM vs 2.13% MM; p< 0.001). Effector CD38+CD81+CD28- NK/T lymphocytes were abundant in MM patients (mean, 2.50% MGUS vs 2.28% SMM vs 4.31% MM; p< 0.05) and CD27- vs CD27+ NK/T lymphocytes ratio augmented during disease progression (p < 0.05). Interestingly, we observed a concomitant reduction of GM-CSF, IFN-α2, IFN-γ, IL-1β, IL-2, IL-2Ra, IL-3, IL-10, IL-13, and MCP-1/CCL2 levels within the BM plasma along MM evolution which could contribute to the myeloid cell decline occurring in these patients. Moreover, PDGF-BB, IFN-α2, IL-16, and IL-8 decrease could be even observed in peripheral blood plasma along MM progression. From a clinical point of view, we evaluated the impact of previously disclosed BM changes on progression-free survival (PFS) of 50 patients with active MM and found that the abundance of granulocytes was associated with a longer PFS (HR: 0.15; p< 0.05). Furthermore, patients treated with daratumumab who had a high BM neutrophil/T lymphocyte ratio showed a substantially longer 1-year PFS (HR: 0.07; p< 0.01) than those who had a low ratio (86% vs 33%, respectively).
Conclusions: Overall, our findings suggest that immune factors play a crucial role in disease development and response to therapy, emphasizing the importance of immune-based approaches for improving patient outcomes in MM.
Methods: We used FlowCT, a semi-automated pipeline for flow cytometry data analysis, to compare the immune composition in the BM of 12 MGUS, 12 SMM, and 63 MM patients stained with two common 8-markers diagnostic tubes. Next, we performed Luminex assays for the simultaneous quantification of 48 cytokines and chemokines using plasma samples of BM and peripheral blood (HD=4, MGUS=12, SMM=12, and MM=12) to obtain a MM immune response profiling.
Results: Progression to clinical MM was associated with a decrease in granulocytes (mean, 74.18% MGUS vs 73.86% SMM vs 65.59% MM; p< 0.05) and an increase in monocytes (mean, 4.97% MGUS vs 4.62% SMM vs 6.77% MM; p< 0.01), T lymphocytes (mean, 6.29% MGUS vs 7.56% SMM vs 11% MM; p< 0.01), and NK cells (mean, 0.88% MGUS vs 1.51% SMM vs 2.13% MM; p< 0.001). Effector CD38+CD81+CD28- NK/T lymphocytes were abundant in MM patients (mean, 2.50% MGUS vs 2.28% SMM vs 4.31% MM; p< 0.05) and CD27- vs CD27+ NK/T lymphocytes ratio augmented during disease progression (p < 0.05). Interestingly, we observed a concomitant reduction of GM-CSF, IFN-α2, IFN-γ, IL-1β, IL-2, IL-2Ra, IL-3, IL-10, IL-13, and MCP-1/CCL2 levels within the BM plasma along MM evolution which could contribute to the myeloid cell decline occurring in these patients. Moreover, PDGF-BB, IFN-α2, IL-16, and IL-8 decrease could be even observed in peripheral blood plasma along MM progression. From a clinical point of view, we evaluated the impact of previously disclosed BM changes on progression-free survival (PFS) of 50 patients with active MM and found that the abundance of granulocytes was associated with a longer PFS (HR: 0.15; p< 0.05). Furthermore, patients treated with daratumumab who had a high BM neutrophil/T lymphocyte ratio showed a substantially longer 1-year PFS (HR: 0.07; p< 0.01) than those who had a low ratio (86% vs 33%, respectively).
Conclusions: Overall, our findings suggest that immune factors play a crucial role in disease development and response to therapy, emphasizing the importance of immune-based approaches for improving patient outcomes in MM.
