Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-254: Cardiac and hidden toxicity of Carfilzomib in presence of Cardiometabolic Syndrome and Early-Stage Heart Failure with reduced Ejection Fraction.
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Panagiotis Efentakis, Dr
PostDoctoral Research
National and Kapodistrian University of Athens
Athens, Greece
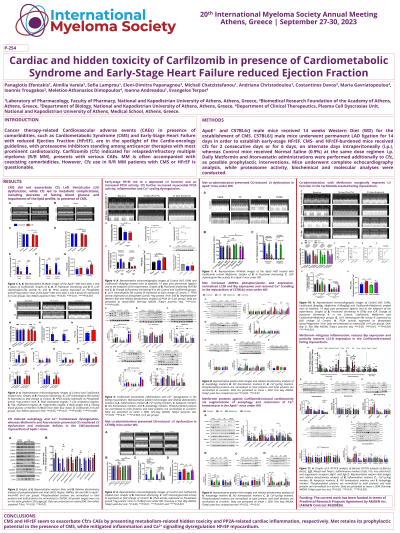
Introduction: Cancer therapy-related Cardiovascular adverse events (CAEs) in presence of comorbidities, such as Cardiometabolic Syndrome (CMS) and Early-Stage Heart Failure with reduced Ejection Fraction (HFrEF), are in the spotlight of the Cardio-oncology guidelines, with proteasome inhibitors standing among anticancer therapies with most prominent cardiotoxicity. Carfilzomib (Cfz) indicated for relapsed/refractory multiple myeloma (MM), presents with serious CAEs. MM is often accompanied with coexisting comorbidities. However, Cfz use in MM patients with CMS or HFrEF is questionable.
Methods: ApoE-/- and C57BL6/J male mice received 14 weeks High Fat Diet (HFD) for the establishment of CMS. C57BL6/J male mice underwent permanent LAD ligation for 14 days in order to establish Early-stage HFrEF. CMS- and HFrEF-burdened mice received Cfz for 2 consecutive days or for 6 days, on alternate days intraperitoneally (i.p.), whereas Control mice received Normal Saline (0.9%) at the same dose regimen i.p. Daily Metformin and Atorvastatin administrations were performed additionally to Cfz, as possible prophylactic interventions. Mice underwent complete echocardiography analysis, while proteasome activity, biochemical and molecular analyses were conducted.
Results: CMS did not exacerbate Cfz Left Ventricular (LV) dysfunction, while Cfz led to metabolic complications, including decrease of fasting blood glucose and impairment of the lipid profile, in both CMS models. Cfz induced autophagy and Ca2+ homeostasis dysregulation, whereas Metformin and Atorvastatin prevented Cfz-mediated LV dysfunction and molecular deficits in the CMS-burdened myocardium. Early-stage HFrEF led to a depressed LV function and an increased PP2A activity. Cfz further increased myocardial PP2A activity, inflammation and Ca2+-cycling dysregulation. Met co-administration exerted an anti-inflammatory potential in the myocardium, without improving LV function.
Conclusions: CMS and HFrEF seem to exacerbate Cfz’s CAEs by presenting metabolism-related hidden toxicity and PP2A-related cardiac inflammation, respectively. Met retains its prophylactic potential in the presence of CMS, while mitigated inflammation and Ca2+ signalling dysregulation HFrEF myocardium.
Methods: ApoE-/- and C57BL6/J male mice received 14 weeks High Fat Diet (HFD) for the establishment of CMS. C57BL6/J male mice underwent permanent LAD ligation for 14 days in order to establish Early-stage HFrEF. CMS- and HFrEF-burdened mice received Cfz for 2 consecutive days or for 6 days, on alternate days intraperitoneally (i.p.), whereas Control mice received Normal Saline (0.9%) at the same dose regimen i.p. Daily Metformin and Atorvastatin administrations were performed additionally to Cfz, as possible prophylactic interventions. Mice underwent complete echocardiography analysis, while proteasome activity, biochemical and molecular analyses were conducted.
Results: CMS did not exacerbate Cfz Left Ventricular (LV) dysfunction, while Cfz led to metabolic complications, including decrease of fasting blood glucose and impairment of the lipid profile, in both CMS models. Cfz induced autophagy and Ca2+ homeostasis dysregulation, whereas Metformin and Atorvastatin prevented Cfz-mediated LV dysfunction and molecular deficits in the CMS-burdened myocardium. Early-stage HFrEF led to a depressed LV function and an increased PP2A activity. Cfz further increased myocardial PP2A activity, inflammation and Ca2+-cycling dysregulation. Met co-administration exerted an anti-inflammatory potential in the myocardium, without improving LV function.
Conclusions: CMS and HFrEF seem to exacerbate Cfz’s CAEs by presenting metabolism-related hidden toxicity and PP2A-related cardiac inflammation, respectively. Met retains its prophylactic potential in the presence of CMS, while mitigated inflammation and Ca2+ signalling dysregulation HFrEF myocardium.
