Treatment of Relapsed/Refractory Myeloma
Poster Session 2
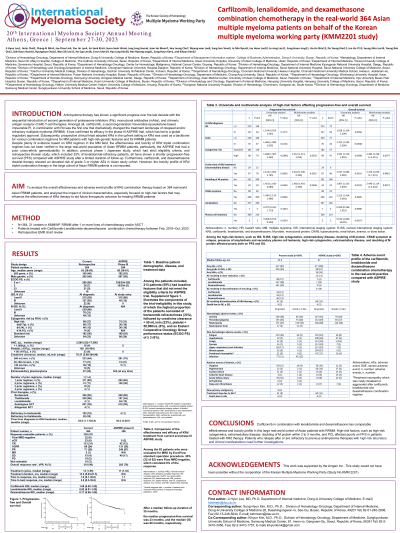
P-284: Carfilzomib, lenalidomide, and dexamethasone combination chemotherapy in the real-world 364 Asian multiple myeloma patients on behalf of the Korean multiple myeloma working party (KMM2201 study)
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST
.jpg)
Ji Hyun Lee (she/her/hers)
Associate professor
Dong-A University College of Medicine
Busan, Republic of Korea
Introduction: Carfilzomib, the second generation proteasome inhibitor (PI), in combination with lenalidomide land dexamethasone (KRd) significantly improved the survival of relapsed and/or refractory multiple myeloma (RRMM) patients. However, the real-world outcome of KRd in a large cohort of Asian MM patient is still lacking. The aim of this study was to analyze the effectiveness and toxicity profile of KRd regimen especially focused on clinical trial eligibility and high-risk clinical factors in Korean RRMM patients outside of the clinical trial.
Methods: Retrospective data of 364 RRMM patients who have received KRd regimen between February, 2018 and October, 2020, was collected from 21 centers participating in the Korean multiple myeloma working party (KMMWP). Clinical trial ineligibility was defined by patient- and treatment-related features that were insufficient to meet the eligibility criteria for ASPIRE trial.
Results: The median age was 63 years (range, 28-85). Forty-nine percent of patients were trial-ineligible. Among the 355 patients whose response were evaluable, overall response rate was 90%, including a very good partial response, a complete response (CR) and a stringent CR of 25%, 32% and 6%. Among the 62 patients who were evaluated for minimal residual disease (MRD) by EuroFlow standard operation procedure, 36% (22 of 62) were Flow MRD-negative. With a median follow-up duration of 34.8 months (range, 0.00-61.5), the median progression-free survival (PFS) and overall survival (OS) were26.4 months (95% confidence interval, CI, 23.1-29.7 months), and not reached. Trial-ineligibility affected to a significant decrease of PFS and OS after KRd treatment . High-risk disease-related factors, high-risk cytogenetics at diagnosis of MM, EMD, doubling of M protein, and symptomatic MM at the time of KRd treatment affected poorly on PFS by univariate and multivariate analysis. Additionally, EMD, doubling of M protein, and symptomatic MM at the time of KRd treatment affected poorly on OS by univariate and multivariate analysis. Hematologic toxicities were more commonly observed than non-hematologic adverse events (AEs). The most common grade 3 or higher toxicities were neutropenia, followed by infections, fatigue, and acute kidney injuries. Grade 3 or higher cardiovascular AEs were observed in less than 5 percent of the patients.
Conclusions: KRd treatment for real-world Korean RRMM patients was highly effective with a tolerable AE profile. Trial-ineligible characteristics and high-risk disease-related features affected poorly to progression-free and overall survival of RRMM patients treated with KRd regimen, which necessitates more effective and tolerable new agents and combination therapies for those patients. This work was supported by Amgen (Grant number: ISS20217193).
Methods: Retrospective data of 364 RRMM patients who have received KRd regimen between February, 2018 and October, 2020, was collected from 21 centers participating in the Korean multiple myeloma working party (KMMWP). Clinical trial ineligibility was defined by patient- and treatment-related features that were insufficient to meet the eligibility criteria for ASPIRE trial.
Results: The median age was 63 years (range, 28-85). Forty-nine percent of patients were trial-ineligible. Among the 355 patients whose response were evaluable, overall response rate was 90%, including a very good partial response, a complete response (CR) and a stringent CR of 25%, 32% and 6%. Among the 62 patients who were evaluated for minimal residual disease (MRD) by EuroFlow standard operation procedure, 36% (22 of 62) were Flow MRD-negative. With a median follow-up duration of 34.8 months (range, 0.00-61.5), the median progression-free survival (PFS) and overall survival (OS) were26.4 months (95% confidence interval, CI, 23.1-29.7 months), and not reached. Trial-ineligibility affected to a significant decrease of PFS and OS after KRd treatment . High-risk disease-related factors, high-risk cytogenetics at diagnosis of MM, EMD, doubling of M protein, and symptomatic MM at the time of KRd treatment affected poorly on PFS by univariate and multivariate analysis. Additionally, EMD, doubling of M protein, and symptomatic MM at the time of KRd treatment affected poorly on OS by univariate and multivariate analysis. Hematologic toxicities were more commonly observed than non-hematologic adverse events (AEs). The most common grade 3 or higher toxicities were neutropenia, followed by infections, fatigue, and acute kidney injuries. Grade 3 or higher cardiovascular AEs were observed in less than 5 percent of the patients.
Conclusions: KRd treatment for real-world Korean RRMM patients was highly effective with a tolerable AE profile. Trial-ineligible characteristics and high-risk disease-related features affected poorly to progression-free and overall survival of RRMM patients treated with KRd regimen, which necessitates more effective and tolerable new agents and combination therapies for those patients. This work was supported by Amgen (Grant number: ISS20217193).
