Other plasma cell disorders
Poster Session 3
P-428: Clinicopathological profile and treatment outcomes in patients with monoclonal gammopathy of renal significance (MGRS): a single centre experience
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Aditya Jandial, MD, DM (Clinical Hematology)
Senior Research Associate
Department of Clinical Hematology, Post Graduate Institute of Medical Education and Research, Chandigarh
Chandigarh, India
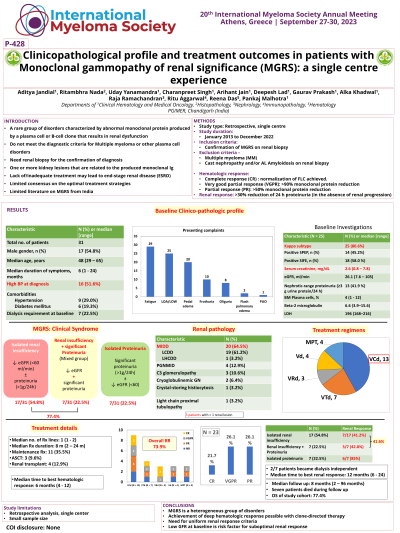
Introduction: Monoclonal gammopathy of renal significance (MGRS) refers to a heterogeneous group of disorders where abnormal monoclonal protein produced by a plasma cell or B-cell clone results in renal dysfunction. These are rare disorders and do not meet diagnostic criteria for other hematologic malignancies. There is limited literature on MGRS from India.
Methods: We performed a retrospective analysis of MGRS patients treated at PGIMER Chandigarh from January 2013 to December 2022. All patients required confirmation of MGRS on renal biopsy for inclusion in the study. Patients with cast nephropathy and renal AL Amyloidosis were excluded. Hematologic response was defined as complete response (CR) if normalization of FLC was achieved. Very good partial response (VGPR) and partial response (PR) required 90% or 50% monoclonal protein reduction, respectively. Renal response was defined as >30% reduction of 24 h proteinuria (in the absence of renal progression).
Results: A total of 31 MGRS patients were analyzed. The median age at diagnosis was 48 years (range 29 – 65 years); 45.2% were females. The median duration of symptoms was 6 months (range 1 – 24 months). Most common presenting complaints were fatigue (82.8%), pedal edema (64.5%), and frothuria (32.2%). At presentation, 20 patients (64.5%) had eGFR < 30 ml/min and 7 patients (22.5%) were on hemodialysis; 16 patients (51.6%) had high blood pressure. Most patients (n = 25, 80.6%) had kappa light chain (LC) disease. Most common renal pathology was monoclonal immunoglobulin deposition disease (MIDD; n = 20, 64.5%), followed by proliferative glomerulonephritis with monoclonal IgG deposits (PGNMID; n = 4, 12.9%), C3 glomerulonephritis (C3GN; n= 3, 10.6%), cryoglobulinemic GN (n = 2, 6.4%), crystal-storing histiocytosis (n = 1; 3.2%) and light chain proximal tubulopathy (n = 1; 3.2%). Three patients had >1 renal lesion on kidney biopsy. Most patients (n = 27; 87.1%) received bortezomib-based first-line therapy; 3 (9.6%) underwent autologous stem cell transplantation. Four patients (12.9%) underwent renal transplantation. The median follow-up duration was 8 months (range 4 - 96 months). The hematologic response was observed in 23/31 patients (74.1%); the median time to best hematologic response was 6 months (range 4-12 months). The renal response was observed in 16/31 patients (51.6%); the median time to best renal response was 12 months (range 6 – 24 months). Normal eGFR at baseline and achievement of CR/VGPR with therapy were independent predictors of renal response. Seven patients died during follow-up. The overall survival (OS) of the study cohort was 77.4%.
Conclusions: These findings suggest that achieving deep hematologic responses with bortezomib-based therapy is crucial to obtaining renal responses in MGRS patients. Low eGFR at baseline is a risk factor for suboptimal renal response.
Methods: We performed a retrospective analysis of MGRS patients treated at PGIMER Chandigarh from January 2013 to December 2022. All patients required confirmation of MGRS on renal biopsy for inclusion in the study. Patients with cast nephropathy and renal AL Amyloidosis were excluded. Hematologic response was defined as complete response (CR) if normalization of FLC was achieved. Very good partial response (VGPR) and partial response (PR) required 90% or 50% monoclonal protein reduction, respectively. Renal response was defined as >30% reduction of 24 h proteinuria (in the absence of renal progression).
Results: A total of 31 MGRS patients were analyzed. The median age at diagnosis was 48 years (range 29 – 65 years); 45.2% were females. The median duration of symptoms was 6 months (range 1 – 24 months). Most common presenting complaints were fatigue (82.8%), pedal edema (64.5%), and frothuria (32.2%). At presentation, 20 patients (64.5%) had eGFR < 30 ml/min and 7 patients (22.5%) were on hemodialysis; 16 patients (51.6%) had high blood pressure. Most patients (n = 25, 80.6%) had kappa light chain (LC) disease. Most common renal pathology was monoclonal immunoglobulin deposition disease (MIDD; n = 20, 64.5%), followed by proliferative glomerulonephritis with monoclonal IgG deposits (PGNMID; n = 4, 12.9%), C3 glomerulonephritis (C3GN; n= 3, 10.6%), cryoglobulinemic GN (n = 2, 6.4%), crystal-storing histiocytosis (n = 1; 3.2%) and light chain proximal tubulopathy (n = 1; 3.2%). Three patients had >1 renal lesion on kidney biopsy. Most patients (n = 27; 87.1%) received bortezomib-based first-line therapy; 3 (9.6%) underwent autologous stem cell transplantation. Four patients (12.9%) underwent renal transplantation. The median follow-up duration was 8 months (range 4 - 96 months). The hematologic response was observed in 23/31 patients (74.1%); the median time to best hematologic response was 6 months (range 4-12 months). The renal response was observed in 16/31 patients (51.6%); the median time to best renal response was 12 months (range 6 – 24 months). Normal eGFR at baseline and achievement of CR/VGPR with therapy were independent predictors of renal response. Seven patients died during follow-up. The overall survival (OS) of the study cohort was 77.4%.
Conclusions: These findings suggest that achieving deep hematologic responses with bortezomib-based therapy is crucial to obtaining renal responses in MGRS patients. Low eGFR at baseline is a risk factor for suboptimal renal response.
