Cellular and T cell engager Immunotherapy
Poster Session 1
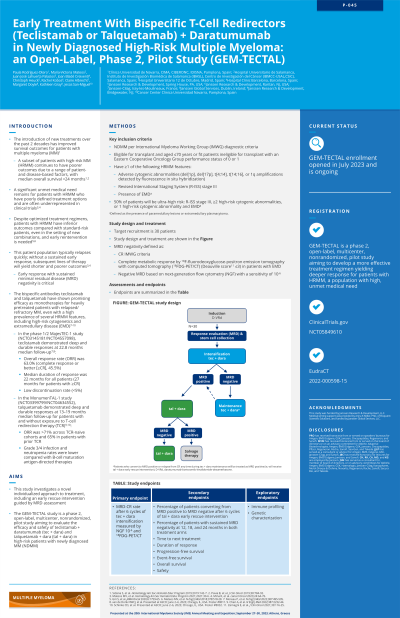
P-045: Early Treatment With Bispecific T-cell Redirectors (Teclistamab or Talquetamab) + Daratumumab in Newly Diagnosed High-risk Multiple Myeloma: An Open-label, Phase 2, Pilot Study (GEM-TECTAL)
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST
.jpg)
Paula Rodríguez-Otero, MD, PhD (she/her/hers)
Associate Professor
Clínica Universidad de Navarra, CIMA, CIBERONC, IDISNA, Pamplona, Spain
Pamplona, Navarra, Spain
Introduction: Trial in progress
Treatment (tx) advancements in recent decades have improved outcomes for patients (pts) with multiple myeloma (MM). However, a subset of pts with high-risk (HR) MM continues to have poor outcomes due to a range of pt- and disease-based factors, with median overall survival (OS) < 24 months. Pts with HRMM have poorly defined treatment options and are often underrepresented in clinical trials; those who fail to achieve MRD negativity after frontline therapy have a particularly high unmet medical need. This phase 2, open-label, multicenter, nonrandomized, pilot study aims to investigate a novel, individualized approach to tx, evaluating the efficacy and safety of teclistamab (tec) + daratumumab (dara) and talquetamab (tal) + dara in pts with HR newly diagnosed (ND) MM, with an early rescue intervention (ERI) guided by MRD assessment.
Methods: Eligible pts are aged ≥18 years with NDMM per International Myeloma Working Group diagnostic criteria, are eligible for transplant and aged ≤70 years, or are fit pts ineligible for transplant with an Eastern Cooperative Oncology Group performance status of 0 or 1. Pts will have ≥1 of the following HRMM features: adverse cytogenic abnormalities (del[17p], t[4;14], t[14;16], or 1q amplifications detected by fluorescence in situ hybridization), Revised International Staging System (R-ISS) stage 3, and presence of extramedullary disease (EMD). 50% of pts will be ultra-high risk: R-ISS stage 3 or “double hit” (≥2 HR cytogenic abnormalities) or 1 HR cytogenic abnormality and EMD.
Induction therapy will consist of dara, bortezomib, lenalidomide, and dexamethasone (D-VRd) and response evaluation, including MRD assessment by multiple techniques. All pts will then receive tec + dara (intensification phase). Following subsequent MRD assessment, pts will be stratified by MRD status. MRD-negative pts will receive tec + dara (maintenance therapy) for a pre-defined period of time. MRD-positive pts will receive tal + dara (ERI) before reassessment. Pts who convert to MRD-negative status will receive tal + dara for a pre-defined period of time; MRD-positive pts will receive salvage therapy. If MRD-negative pts convert to MRD-positive status, they will be treated as MRD-positive pts. The primary endpoint is MRD-complete response rate after tx with tec + dara (intensification). Secondary endpoints include percentage of pts who convert to MRD negativity after ERI; percentage of pts with sustained MRD negativity at pre-defined time points in both tx arms; OS; progression-free survival; event-free survival; time to next tx; duration of response; and safety. Exploratory endpoints are immune profiling and genetic characterization.
Results: Enrollment is expected to begin in May 2023 (target recruitment N=30).
Conclusions: This study will provide needed data on the effect of MRD-guided individualized tx approaches in management of pts with HRMM, an underrepresented population with a high unmet need.
Treatment (tx) advancements in recent decades have improved outcomes for patients (pts) with multiple myeloma (MM). However, a subset of pts with high-risk (HR) MM continues to have poor outcomes due to a range of pt- and disease-based factors, with median overall survival (OS) < 24 months. Pts with HRMM have poorly defined treatment options and are often underrepresented in clinical trials; those who fail to achieve MRD negativity after frontline therapy have a particularly high unmet medical need. This phase 2, open-label, multicenter, nonrandomized, pilot study aims to investigate a novel, individualized approach to tx, evaluating the efficacy and safety of teclistamab (tec) + daratumumab (dara) and talquetamab (tal) + dara in pts with HR newly diagnosed (ND) MM, with an early rescue intervention (ERI) guided by MRD assessment.
Methods: Eligible pts are aged ≥18 years with NDMM per International Myeloma Working Group diagnostic criteria, are eligible for transplant and aged ≤70 years, or are fit pts ineligible for transplant with an Eastern Cooperative Oncology Group performance status of 0 or 1. Pts will have ≥1 of the following HRMM features: adverse cytogenic abnormalities (del[17p], t[4;14], t[14;16], or 1q amplifications detected by fluorescence in situ hybridization), Revised International Staging System (R-ISS) stage 3, and presence of extramedullary disease (EMD). 50% of pts will be ultra-high risk: R-ISS stage 3 or “double hit” (≥2 HR cytogenic abnormalities) or 1 HR cytogenic abnormality and EMD.
Induction therapy will consist of dara, bortezomib, lenalidomide, and dexamethasone (D-VRd) and response evaluation, including MRD assessment by multiple techniques. All pts will then receive tec + dara (intensification phase). Following subsequent MRD assessment, pts will be stratified by MRD status. MRD-negative pts will receive tec + dara (maintenance therapy) for a pre-defined period of time. MRD-positive pts will receive tal + dara (ERI) before reassessment. Pts who convert to MRD-negative status will receive tal + dara for a pre-defined period of time; MRD-positive pts will receive salvage therapy. If MRD-negative pts convert to MRD-positive status, they will be treated as MRD-positive pts. The primary endpoint is MRD-complete response rate after tx with tec + dara (intensification). Secondary endpoints include percentage of pts who convert to MRD negativity after ERI; percentage of pts with sustained MRD negativity at pre-defined time points in both tx arms; OS; progression-free survival; event-free survival; time to next tx; duration of response; and safety. Exploratory endpoints are immune profiling and genetic characterization.
Results: Enrollment is expected to begin in May 2023 (target recruitment N=30).
Conclusions: This study will provide needed data on the effect of MRD-guided individualized tx approaches in management of pts with HRMM, an underrepresented population with a high unmet need.
