Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-307: Efficacy and safety of elranatamab monotherapy in patients with relapsed/refractory multiple myeloma: A post-hoc subgroup analysis from MagnetisMM-3 with modified eligibility criteria
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Marc S. Raab, MD PhD
Professor of Medicine
Dept. of Medicine V Hematology, Oncology and Rheumatology, University Hospital Heidelberg, Heidelberg, Germany
Heidelberg, Germany
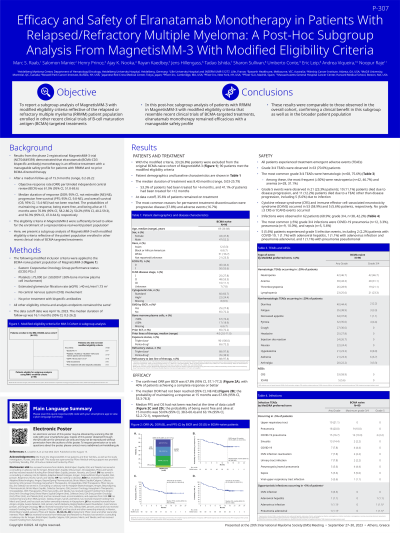
Introduction: Results from the Phase 2 MagnetisMM-3 trial (NCT04649359) demonstrated elranatamab (BCMA x CD3 bispecific monoclonal antibody [bsAb]) monotherapy as an effective treatment for patients (pts) with RRMM with a manageable safety profile. Eligibility criteria in MagnetisMM-3 were sufficiently broad to allow for the enrollment of a representative real-world pt population. Here, we present a subgroup analysis of MagnetisMM-3 with modified eligibility criteria reflective of the pt population enrolled in other recent clinical trials of BCMA-directed bsAb.
Methods: The following modified inclusion/exclusion criteria were applied to the pt population of MagnetisMM-3 Cohort A (BCMA-naïve): ECOG PS ≤1, no CNS involvement, no prior treatment with bi-specific antibodies, platelets ≥75,000 (or ≥50,000 if ≥50% bone marrow plasma cell involvement), eGFR ≥40 mL/min/1.73 m^2. All other eligibility criteria and analysis endpoints remained the same as previously reported (Bahlis et al., ASH 2022). Data cutoff was ~15 mo after last pt’s initial dose.
Results: With the modified criteria, 33 (26.8%) pts were excluded from the original analysis population of MagnetisMM-3 Cohort A. For the 90 pts meeting the modified eligibility criteria, median age was 69 y (range, 36−88), 52.2% were male; median number of prior lines of therapy was 4.0 (2−11); 97.8% and 38.9% of pts were triple-class- and penta-drug refractory, respectively. High-risk cytogenetics [t(4;14), t(14;16),or del(17p)] were present in 24.4% of pts, 27.8% of pts had extramedullary disease by BICR and 11.1% had an R-ISS of III at baseline.
At data cutoff, the median follow-up was 15.1 mo (range, 0.2–25.1) and the median treatment duration was 8.4 mo (range, 0.03–24.4); 36.7% of pts remained on treatment. Most common reason for permanent treatment discontinuation was progressive disease (37.8%). Objective response rate per BICR was 67.8% (95% CI, 57.1, 77.2), with 38.9% CR or sCR, 24.4% VGPR, and 4.4% PR. Median duration of response (DOR) has not been reached (95% CI, NE−NE) and DOR rate at 15 mo was 67.1% (95% CI, 52.7, 78.0), median progression-free survival was 13.9 mo (95% CI, 9.8, NE). Most common Grade 3/4 treatment-emergent AEs were hematologic (75.6%), among these the most frequent (≥30%) were neutropenia (46.7%) and anemia (31.1%). Grade 3/4 infections were reported in 41.1% of pts, most common (≥10%) was COVID-19 pneumonia (13.3%); 5 (5.6%) pts had Grade 5 infections. CRS and ICANS occurred in 58.9% and 5.6% of pts respectively. There were no Grade ≥3 CRS or ICANS events.
Conclusions: In this post-hoc subgroup analysis of pts with RRMM in MagnetisMM-3 with modified eligibility criteria that resemble recent clinical trials of BCMA-directed bsAb, elranatamab monotherapy remained efficacious with a manageable safety profile. Results were comparable to those observed in the overall cohort confirming a clinical benefit in this subgroup as well as in the overall broader pt population.
Methods: The following modified inclusion/exclusion criteria were applied to the pt population of MagnetisMM-3 Cohort A (BCMA-naïve): ECOG PS ≤1, no CNS involvement, no prior treatment with bi-specific antibodies, platelets ≥75,000 (or ≥50,000 if ≥50% bone marrow plasma cell involvement), eGFR ≥40 mL/min/1.73 m^2. All other eligibility criteria and analysis endpoints remained the same as previously reported (Bahlis et al., ASH 2022). Data cutoff was ~15 mo after last pt’s initial dose.
Results: With the modified criteria, 33 (26.8%) pts were excluded from the original analysis population of MagnetisMM-3 Cohort A. For the 90 pts meeting the modified eligibility criteria, median age was 69 y (range, 36−88), 52.2% were male; median number of prior lines of therapy was 4.0 (2−11); 97.8% and 38.9% of pts were triple-class- and penta-drug refractory, respectively. High-risk cytogenetics [t(4;14), t(14;16),or del(17p)] were present in 24.4% of pts, 27.8% of pts had extramedullary disease by BICR and 11.1% had an R-ISS of III at baseline.
At data cutoff, the median follow-up was 15.1 mo (range, 0.2–25.1) and the median treatment duration was 8.4 mo (range, 0.03–24.4); 36.7% of pts remained on treatment. Most common reason for permanent treatment discontinuation was progressive disease (37.8%). Objective response rate per BICR was 67.8% (95% CI, 57.1, 77.2), with 38.9% CR or sCR, 24.4% VGPR, and 4.4% PR. Median duration of response (DOR) has not been reached (95% CI, NE−NE) and DOR rate at 15 mo was 67.1% (95% CI, 52.7, 78.0), median progression-free survival was 13.9 mo (95% CI, 9.8, NE). Most common Grade 3/4 treatment-emergent AEs were hematologic (75.6%), among these the most frequent (≥30%) were neutropenia (46.7%) and anemia (31.1%). Grade 3/4 infections were reported in 41.1% of pts, most common (≥10%) was COVID-19 pneumonia (13.3%); 5 (5.6%) pts had Grade 5 infections. CRS and ICANS occurred in 58.9% and 5.6% of pts respectively. There were no Grade ≥3 CRS or ICANS events.
Conclusions: In this post-hoc subgroup analysis of pts with RRMM in MagnetisMM-3 with modified eligibility criteria that resemble recent clinical trials of BCMA-directed bsAb, elranatamab monotherapy remained efficacious with a manageable safety profile. Results were comparable to those observed in the overall cohort confirming a clinical benefit in this subgroup as well as in the overall broader pt population.
