Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-295: Efficacy, Survival and Safety of Selinexor, Bortezomib and Dexamethasone (SVd) in Patients with Lenalidomide-Refractory Multiple Myeloma: Subgroup Data from the BOSTON Trial
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

María-Victoria Mateos, MD, PhD
Professor
University Hospital of Salamanca/IBSAL/CIC/CIBERONC, Salamanca, Spain
Salamanca, Spain
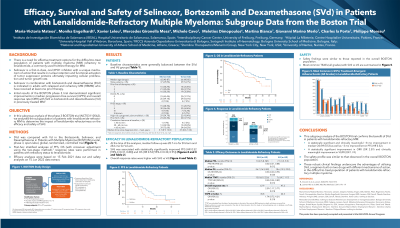
Introduction: Lenalidomide (LEN) is commonly used in frontline therapy for newly diagnosed MM, and there is a need for effective treatment options for patients (pts) with MM refractory to LEN. Selinexor is a first-in-class, oral XPO1 inhibitor with a unique mechanism of action. SVd is indicated in adults with relapsed and refractory MM (RRMM) who have received at least one prior therapy. Initial results of the BOSTON phase 3 trial demonstrated significant improvements in median progression-free survival (mPFS) and overall response rate (ORR) with SVd vs bortezomib and dexamethasone (Vd) in previously treated MM (Grosicki et al. Lancet 2020). We analyzed data from the phase 3 BOSTON trial (NCT03110562) to determine the impact of refractoriness to LEN on SVd efficacy (both PFS and overall survival [OS]) and safety.
Methods: Eligible pts with RRMM and 1-3 prior therapies were randomized to SVd (selinexor 100 mg QW, bortezomib 1.3 mg/m2 QW and dexamethasone 20 mg BIW) or standard Vd BIW. We performed a post-hoc stratified analysis of PFS, OS (with crossover adjustment using the two-stage method), response rates and safety in subgroups by refractory status to LEN.
Results: Of 402 pts, 106 were classified as LEN-refractory (SVd=53, Vd=53). Sixteen pts (30.2%) in the SVd arm became LEN-refractory after 1 prior line of therapy (LOT) and 69.8% after 2 or more LOT; in the Vd group 26.4% became LEN-refractory after 1 prior LOT; 73.6% after 2 or more LOT. Median age was 65 ys (range 40-87) in the SVd arm and 66 y (range 45-85) in the Vd arm. At the time of the analyses, median follow-up was 28.7 mo for SVd arm and 28.6 mo for Vd arm. mPFS was 10.2 mo (95% CI 5.8-NR) with SVd vs 7.1 mo (95% CI 3.5-9.8) with Vd (HR 0.52; 95% CI 0.31-0.88, p=0.012). mOS was 26.7 mo (95% CI 19.9-NR) with SVd vs 18.6 mo (95% CI 13.9-29.0) with Vd, resulting in a statistically significant and clinically meaningful improvement in OS (HR 0.53; 95% CI 0.30-0.95, p=0.03). Response rates for SVd and Vd were as follows: ORR 67.9% vs 47.2% and VGPR or better 35.8% vs 24.5%, respectively. The most common (≥25%) treatment-emergent adverse events with SVd vs Vd in 105 LEN-refractory pts included in the safety population were thrombocytopenia (71.7% vs 40.4%), nausea (50.9% vs 11.5%), fatigue (45.3% vs 21.1%), diarrhea (43.4% vs 19.2%), anemia (39.6% vs 25.0%), and peripheral neuropathy (30.2% vs 38.5%).
Conclusions: Subgroup data from the BOSTON trial show a statistically significant and clinically meaningful improvement in OS and PFS and higher ORR and VGPR or better with SVd vs Vd in LEN-refractory RRMM pts. The safety profile in the subgroups was similar to that observed in the overall BOSTON population. The statistically significant 47% reduction in risk of death with SVd vs Vd shows an advantage of having a regimen built on two drugs with different mechanisms of action in the difficult-to-treat population of LEN-refractory RRMM pts.
Methods: Eligible pts with RRMM and 1-3 prior therapies were randomized to SVd (selinexor 100 mg QW, bortezomib 1.3 mg/m2 QW and dexamethasone 20 mg BIW) or standard Vd BIW. We performed a post-hoc stratified analysis of PFS, OS (with crossover adjustment using the two-stage method), response rates and safety in subgroups by refractory status to LEN.
Results: Of 402 pts, 106 were classified as LEN-refractory (SVd=53, Vd=53). Sixteen pts (30.2%) in the SVd arm became LEN-refractory after 1 prior line of therapy (LOT) and 69.8% after 2 or more LOT; in the Vd group 26.4% became LEN-refractory after 1 prior LOT; 73.6% after 2 or more LOT. Median age was 65 ys (range 40-87) in the SVd arm and 66 y (range 45-85) in the Vd arm. At the time of the analyses, median follow-up was 28.7 mo for SVd arm and 28.6 mo for Vd arm. mPFS was 10.2 mo (95% CI 5.8-NR) with SVd vs 7.1 mo (95% CI 3.5-9.8) with Vd (HR 0.52; 95% CI 0.31-0.88, p=0.012). mOS was 26.7 mo (95% CI 19.9-NR) with SVd vs 18.6 mo (95% CI 13.9-29.0) with Vd, resulting in a statistically significant and clinically meaningful improvement in OS (HR 0.53; 95% CI 0.30-0.95, p=0.03). Response rates for SVd and Vd were as follows: ORR 67.9% vs 47.2% and VGPR or better 35.8% vs 24.5%, respectively. The most common (≥25%) treatment-emergent adverse events with SVd vs Vd in 105 LEN-refractory pts included in the safety population were thrombocytopenia (71.7% vs 40.4%), nausea (50.9% vs 11.5%), fatigue (45.3% vs 21.1%), diarrhea (43.4% vs 19.2%), anemia (39.6% vs 25.0%), and peripheral neuropathy (30.2% vs 38.5%).
Conclusions: Subgroup data from the BOSTON trial show a statistically significant and clinically meaningful improvement in OS and PFS and higher ORR and VGPR or better with SVd vs Vd in LEN-refractory RRMM pts. The safety profile in the subgroups was similar to that observed in the overall BOSTON population. The statistically significant 47% reduction in risk of death with SVd vs Vd shows an advantage of having a regimen built on two drugs with different mechanisms of action in the difficult-to-treat population of LEN-refractory RRMM pts.
