Myeloma Genomics and cell signaling
Poster Session 3
P-334: Fluorescence in situ hybridization (FISH) t(11;14) testing practices over time in patients with newly diagnosed multiple myeloma (MM) in the USA in the Flatiron Health database
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Linda B. Baughn, PhD (she/her/hers)
Co-director, Cytogenetics Laboratory/Consultant
Mayo Clinic, Rochester, MN, US, Minnesota, United States
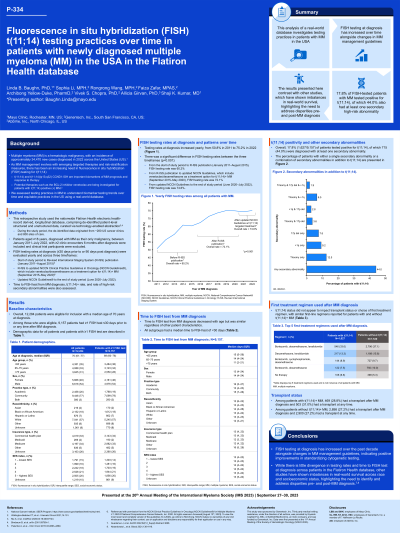
Introduction: t(11;14) is an important biomarker of MM prognosis and response to therapy, including the BCL-2 inhibitor venetoclax. As MM management evolves with emerging targeted therapies and risk-stratification measures, FISH testing for t(11;14) is needed. We assessed testing practices in MM to understand biomarker testing trends and equitable practices in the USA using the Flatiron Health database.
Methods: This retrospective study included patients aged ≥ 18 years, diagnosed with MM as their first and only malignancy in the nationwide Flatiron Health electronic health-record derived, de-identified database, between January 2011–July 2022, with ≥ 2 clinic encounters 6 months after diagnosis. Clinical trial participants were excluded. FISH testing rates at diagnosis (≤ 30 days prior to or 90 days post-diagnosis) were evaluated across three timeframes: start of study period to R-ISS publication (Palumbo et al. 2015) (January 2011–August 2015), R-ISS to updated NCCN guidelines (V.1.2020) which include venetoclax for t(11;14)+ MM (September 2015–May 2020), and updated NCCN guidelines to end of study period (June 2020–July 2022). Time to FISH test from diagnosis was assessed.
Results: Amongst 12,284 eligible patients, at diagnosis, median (interquartile range [IQR]) age was 70 (61–77) years, 46% were female, and 68.8% (n = 8,451) had a FISH test. Testing rates at diagnosis increased yearly, from 50.1% in 2011 to 75.1% by 2022, and during the three defined timeframes (starting from earliest) were 60.2%, 72.1%, and 74.6% (p < 0.001). For FISH tests beyond diagnosis (≤ 30 days prior or any time post-diagnosis), 75% (n = 9,157) had ≥ 1 test and median (IQR) time to test was 13 (4–24) days.
Testing rates were similar regardless of care setting (community/academic), race/ethnicity, gender, and socioeconomic status index, but decreased with older age ( < 65 years: 80.1% [n = 3,484/4,351], 65–75 years: 76.4% [n = 3,123/4,088], > 75 years: 66.3% [n = 2,550/3,845]). All subgroups had a median time from diagnosis to FISH test of < 30 days.
Despite 17.8% (n = 1,627/9,157) of tested patients having t(11;14), first treatment choice was not impacted, with similar first-line regimens reported for patients with/without t(11;14).
Conclusions: FISH testing at diagnosis has increased since 2011 alongside changes in MM management guidelines. Though the Flatiron Health database shows minimal testing disparities, other studies indicate real-world survival imbalances; thus there is still a need to identify and address disparities pre- and post-MM diagnosis.
Methods: This retrospective study included patients aged ≥ 18 years, diagnosed with MM as their first and only malignancy in the nationwide Flatiron Health electronic health-record derived, de-identified database, between January 2011–July 2022, with ≥ 2 clinic encounters 6 months after diagnosis. Clinical trial participants were excluded. FISH testing rates at diagnosis (≤ 30 days prior to or 90 days post-diagnosis) were evaluated across three timeframes: start of study period to R-ISS publication (Palumbo et al. 2015) (January 2011–August 2015), R-ISS to updated NCCN guidelines (V.1.2020) which include venetoclax for t(11;14)+ MM (September 2015–May 2020), and updated NCCN guidelines to end of study period (June 2020–July 2022). Time to FISH test from diagnosis was assessed.
Results: Amongst 12,284 eligible patients, at diagnosis, median (interquartile range [IQR]) age was 70 (61–77) years, 46% were female, and 68.8% (n = 8,451) had a FISH test. Testing rates at diagnosis increased yearly, from 50.1% in 2011 to 75.1% by 2022, and during the three defined timeframes (starting from earliest) were 60.2%, 72.1%, and 74.6% (p < 0.001). For FISH tests beyond diagnosis (≤ 30 days prior or any time post-diagnosis), 75% (n = 9,157) had ≥ 1 test and median (IQR) time to test was 13 (4–24) days.
Testing rates were similar regardless of care setting (community/academic), race/ethnicity, gender, and socioeconomic status index, but decreased with older age ( < 65 years: 80.1% [n = 3,484/4,351], 65–75 years: 76.4% [n = 3,123/4,088], > 75 years: 66.3% [n = 2,550/3,845]). All subgroups had a median time from diagnosis to FISH test of < 30 days.
Despite 17.8% (n = 1,627/9,157) of tested patients having t(11;14), first treatment choice was not impacted, with similar first-line regimens reported for patients with/without t(11;14).
Conclusions: FISH testing at diagnosis has increased since 2011 alongside changes in MM management guidelines. Though the Flatiron Health database shows minimal testing disparities, other studies indicate real-world survival imbalances; thus there is still a need to identify and address disparities pre- and post-MM diagnosis.
