Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-317: How do patients and providers value innovative multiple myeloma treatments? Evidence from a discrete choice experiment
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Sakil Syeed, MBBS (he/him/his)
HEOR Graduate Research Assistant, Ph.D. candidate
University of Utah College of Pharmacy, Salt Lake City, UT
Salt Lake City, Utah, United States
Introduction: Survival improvement for patients (pts) with multiple myeloma (MM) is attributed to innovative treatments (Tx). The impact of these innovative Tx is generally measured through disease improvement and pt survival; however, the value ascribed to innovation remains unclear. Understanding pt and healthcare provider (HCP) preferences for innovation can help support shared decision-making and improve pt outcomes. This study aimed to investigate pt and HCP preferences for innovative MM Tx.
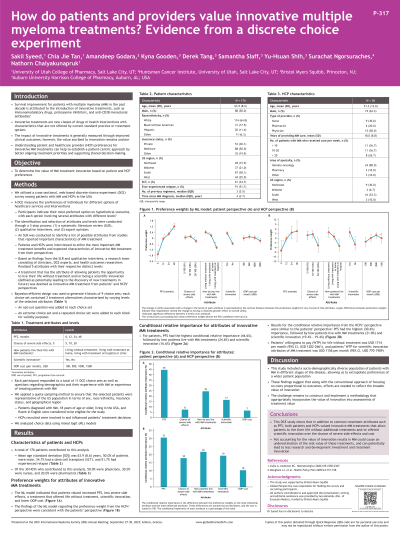
Methods: This mixed methods research study leveraged qualitative and quantitative approaches to understand perspectives among pts with MM and HCPs regarding the value of innovation in MM. A literature review, followed by interviews with pts and HCPs, were conducted to identify treatment attributes, and 5 attributes were selected. Tx alternatives were characterized by varying levels of (1) progression-free survival (PFS: 6, 12, 24, 48 months); (2) probability of severe side effects (5%, 10%, 20%); (3) how pts live with MM Tx (living without Tx, living with Tx at home, living with Tx at a hospital); (4) scientific innovation, defined as a Tx that is either first-in-class or leads to future development of better MM Tx (yes, no); and (5) monthly OOP cost ($100, $500, $1000, $1500). A Tx that provides the opportunity to live without Tx and/or offers scientific innovation was deemed innovative. Subsequently, discrete choice experiment surveys were conducted. Choice data were analyzed using mixed logit (ML) models.
Results: Forty-seven pts participated in this interim analysis. The average age was 62.4 years; most were female (n=29, 62%) and had experienced relapse (n=30, 64%). The ML model revealed that pts preferred increased PFS, less severe side effects, a Tx that offered life without Tx, scientific innovation, and lower OOP cost. PFS had the highest conditional relative importance (37%) from the pts' perspective, followed by the OOP cost (27%) and how they live with MM Tx (17%).
Of the 30 HCPs, 50% were physicians (n=15), 30% were nurses (n=9), and 20% were pharmacists (n=6). The findings of the ML model were consistent with the pt survey. PFS had the highest conditional relative importance from the HCPs’ perspective (31%), followed by how pts live with MM Tx (22%) and scientific innovation (19%).
Conclusions: Our findings show that pts and HCPs positively valued innovative MM Tx that provided the opportunity to live without Tx and/or offered scientific innovation. Not accounting for the value of innovation would result in underestimation of its value and potentially lead to less access to innovation and less R&D investment for future innovation.
Methods: This mixed methods research study leveraged qualitative and quantitative approaches to understand perspectives among pts with MM and HCPs regarding the value of innovation in MM. A literature review, followed by interviews with pts and HCPs, were conducted to identify treatment attributes, and 5 attributes were selected. Tx alternatives were characterized by varying levels of (1) progression-free survival (PFS: 6, 12, 24, 48 months); (2) probability of severe side effects (5%, 10%, 20%); (3) how pts live with MM Tx (living without Tx, living with Tx at home, living with Tx at a hospital); (4) scientific innovation, defined as a Tx that is either first-in-class or leads to future development of better MM Tx (yes, no); and (5) monthly OOP cost ($100, $500, $1000, $1500). A Tx that provides the opportunity to live without Tx and/or offers scientific innovation was deemed innovative. Subsequently, discrete choice experiment surveys were conducted. Choice data were analyzed using mixed logit (ML) models.
Results: Forty-seven pts participated in this interim analysis. The average age was 62.4 years; most were female (n=29, 62%) and had experienced relapse (n=30, 64%). The ML model revealed that pts preferred increased PFS, less severe side effects, a Tx that offered life without Tx, scientific innovation, and lower OOP cost. PFS had the highest conditional relative importance (37%) from the pts' perspective, followed by the OOP cost (27%) and how they live with MM Tx (17%).
Of the 30 HCPs, 50% were physicians (n=15), 30% were nurses (n=9), and 20% were pharmacists (n=6). The findings of the ML model were consistent with the pt survey. PFS had the highest conditional relative importance from the HCPs’ perspective (31%), followed by how pts live with MM Tx (22%) and scientific innovation (19%).
Conclusions: Our findings show that pts and HCPs positively valued innovative MM Tx that provided the opportunity to live without Tx and/or offered scientific innovation. Not accounting for the value of innovation would result in underestimation of its value and potentially lead to less access to innovation and less R&D investment for future innovation.
