Treatment of Newly Diagnosed Myeloma - Transplant Eligible
Poster Session 1
P-157: How public policies have improved the overall survival of transplant eligible newly diagnosed multiple myeloma patients in the Chilean public health system
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Camila Peña, MD
Hematologist
Hospital del Salvador, Santiago de Chile
Santiago, Chile
Introduction: In Chile, particularly in the public system, treatment of patients with transplant eligible NDMM has evolved, being divided into 4 treatment periods endorsed and financed by the Ministry of Health, since 2000.
The main aim of this study was to evaluate the overall survival (OS) of these patients in the different periods.
Methods: Ambispective observational cohort study. A total of 213 ≤65 years patients from our institutional registry were analyzed. Since 2013 the registry is prospective. Four periods were defined: 1 (P1) from 2000 to 2007, in which there was only melphalan-prednisone as treatment; Period 2 (P2) from 2008 to 2013, in which thalidomide began to be used for some young patients, in addition to autologous stem cell transplantation (ASCT) in some cases; Period 3 (P3) from 2014 to 2018, in which the protocol to be used was cyclophosphamide-thalidomide-dexamethasone (CTD) and ASCT; Period 4 (P4) from 2019 to 2022, in which triplets based on bortezomib, ASCT and post-transplant maintenance with lenalidomide were used. The indications for ASCT in all periods were restrictive: Only for patients ≤60 years in very good partial response (VGPR) or better.
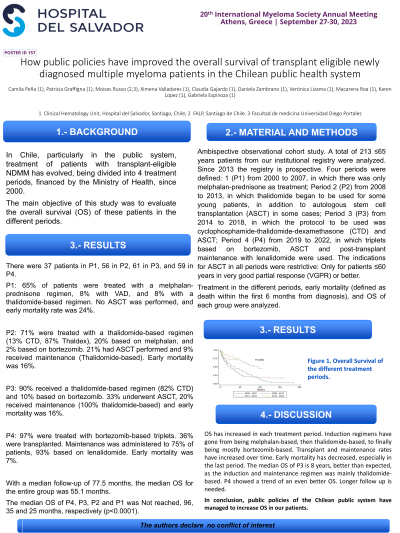
Treatment in the different periods, early mortality (defined as death within the first 6 months of diagnosis), and OS of each group were analyzed.
Results: There were 37 patients at P1, 56 at P2, 61 at P3, and 59 at P4.
At P1, 65% of patients were treated with a melphalan-prednisone regimen, 8% VAD, and 8% with a thalidomide-based regimen. No ASCT was performed, and early mortality rate was 24%.
At P2, 71% were treated with a thalidomide-based regimen (13% CTD, 87% Thaldex), 20% based on melphalan, and 2% based on bortezomib. 21% had ASCT performed and 9% received maintenance (Thalidomide-based). Early mortality was 16%.
At P3, 90% received a thalidomide-based regimen (82% CTD) and 10% based on bortezomib. 33% underwent ASCT, 20% received maintenance (100% thalidomide-based) and early mortality was 16%.
At P4, 97% were treated with bortezomib-based triplets. 36% were transplanted. Maintenance was administered to 75% of patients, 93% based on lenalidomide. Early mortality was 7%.
With a median follow-up of 77.5 months, the median OS for the entire group was 55.1 months.
The median OS of P4, P3, P2 and P1 was Not reached, 96, 35 and 25 months, respectively (p < 0.0001).
Conclusions: OS has increased in each treatment period. Induction regimens have gone from being melphalan-based, then thalidomide-based, to finally being mostly bortezomib-based. Transplant and maintenance rates have increased over time. Early mortality has decreased, especially in the last period. The median OS of P3 is 8 years, better than expected, as the induction and maintenance regimen was mainly thalidomide-based. P4 showed a trend of an even better OS. Longer follow up is needed.
In conclusion, public policies in the Chilean public system have managed to increase OS in our patients.
The main aim of this study was to evaluate the overall survival (OS) of these patients in the different periods.
Methods: Ambispective observational cohort study. A total of 213 ≤65 years patients from our institutional registry were analyzed. Since 2013 the registry is prospective. Four periods were defined: 1 (P1) from 2000 to 2007, in which there was only melphalan-prednisone as treatment; Period 2 (P2) from 2008 to 2013, in which thalidomide began to be used for some young patients, in addition to autologous stem cell transplantation (ASCT) in some cases; Period 3 (P3) from 2014 to 2018, in which the protocol to be used was cyclophosphamide-thalidomide-dexamethasone (CTD) and ASCT; Period 4 (P4) from 2019 to 2022, in which triplets based on bortezomib, ASCT and post-transplant maintenance with lenalidomide were used. The indications for ASCT in all periods were restrictive: Only for patients ≤60 years in very good partial response (VGPR) or better.
Treatment in the different periods, early mortality (defined as death within the first 6 months of diagnosis), and OS of each group were analyzed.
Results: There were 37 patients at P1, 56 at P2, 61 at P3, and 59 at P4.
At P1, 65% of patients were treated with a melphalan-prednisone regimen, 8% VAD, and 8% with a thalidomide-based regimen. No ASCT was performed, and early mortality rate was 24%.
At P2, 71% were treated with a thalidomide-based regimen (13% CTD, 87% Thaldex), 20% based on melphalan, and 2% based on bortezomib. 21% had ASCT performed and 9% received maintenance (Thalidomide-based). Early mortality was 16%.
At P3, 90% received a thalidomide-based regimen (82% CTD) and 10% based on bortezomib. 33% underwent ASCT, 20% received maintenance (100% thalidomide-based) and early mortality was 16%.
At P4, 97% were treated with bortezomib-based triplets. 36% were transplanted. Maintenance was administered to 75% of patients, 93% based on lenalidomide. Early mortality was 7%.
With a median follow-up of 77.5 months, the median OS for the entire group was 55.1 months.
The median OS of P4, P3, P2 and P1 was Not reached, 96, 35 and 25 months, respectively (p < 0.0001).
Conclusions: OS has increased in each treatment period. Induction regimens have gone from being melphalan-based, then thalidomide-based, to finally being mostly bortezomib-based. Transplant and maintenance rates have increased over time. Early mortality has decreased, especially in the last period. The median OS of P3 is 8 years, better than expected, as the induction and maintenance regimen was mainly thalidomide-based. P4 showed a trend of an even better OS. Longer follow up is needed.
In conclusion, public policies in the Chilean public system have managed to increase OS in our patients.
