Myeloma Genomics and cell signaling
Poster Session 3
P-359: Non-Paraskeletal Extramedullary Disease Is Associated with high rates of high risk cytogenetic alterations and has a distinct transcriptional profile
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Mateo Mejia Saldarriaga, MD
Assistan Professor
Weill Cornell Medicine
New York, New York, United States
Introduction: Extramedullary disease (EMD) is seen in up to a third of patients during multiple myeloma (MM) courses, and it is associated with worse outcomes (overall survival (OS) and progression-free survival (PFS)) despite the upfront use of autologous stem cell transplant (ASCT), proteasome inhibitor, and immunomodulatory drugs combination. However, molecular drivers of EMD are poorly characterized.
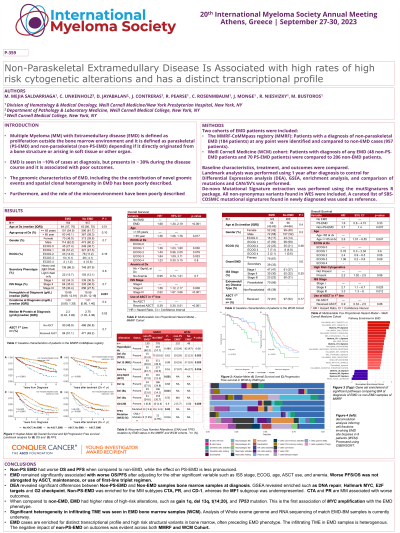
Methods: A 124-patient cohort with EMD (70 paraskeletal (PS) and 48 non-paraskeletal (non-PS)) from a single institution (Weill Cornell, WCM) were compared to a randomly selected non-EMD MM control group (232 patients). The MM Research Foundation (MMRF) CoMMpass registry was queried, and patients who developed non-PS EMD (184 patients) at any point were compared to non-EMD group (957 patients). Baseline characteristics and clinical outcomes were compared. Copy number alterations, structural variants, point mutations, differential expression analysis (DEA) and mutational signature were compared in the MMRF cohort from the sample at diagnosis. Analysis of Whole exome and RNA sequencing of 8 matched bone marrow-EMD biopsies is currently underway and will be available at the meeting.
Results: EMD is associated with lower M protein (p = 0.02) and higher hemoglobin (p < 0.01) at diagnosis in the MMRF. Lower OS (WCM: HR 3.4, CI 1.5-7.9 p < 0.01, MMRF: HR 1.5, CI 1.2-1.9, p = 0.018) and PFS (MMRF: HR 1.51, 95CI (1.23 - 1.87), p < 0.01) were seen in non-PS EMD after adjusting for ASCT use, presence of anemia, LDH, ISS, and high-risk cytogenetics. The use of ASCT, maintenance, and triplet induction led to improved outcomes, but the effect of EMD was not abrogated. Landmark analysis was performed in the MMRF for ASCT and maintenance with similar results.
Non-PS EMD was associated with higher rates of del17p (WCM 29% vs 14%, p 0.02), TP53 mutations (MMRF 9.6% vs 4.4%, p 0.02) and biallelic TP53 inactivation (MMRF 7.3% vs 2.9%, p 0.01), gain 1q (MMRF 44% vs 37%, WCM 47% vs 27%, p 0.01), del13q (WCM 53% vs 33%, p 0.02), Amp 8q24 (MYC, MMRF 27% vs 15%, p < 0.01) and del18q (MMRF 23% vs 14%, p < 0.01) when compared to non-EMD cases. There were no differences in mutations in top 25 recurrent genes. DEA and GSEA showed enrichment of the MYC target, E2F, G2M checkpoint pathways, and of the CD-1 (CCND1), CTA (cancer testis antigen), and PR (proliferative) myeloma subgroups, while there was lower expression of the focal adhesion molecules (FAC) pathway, MS, MF, and LB myeloma subgroups non-EMD samples. There were no differences in tumor mutation burden or selected COSMIC signature frequency between EMD and non-EMD samples.
Conclusions: Non-PS EMD is associated with worse clinical outcomes, with higher incidence of known high-risk molecular alterations (del17p, gain1q), in addition to other not previously identified such as amp8q24 (MYC). This correlates with enrichment for MYC and lower expression of FAC pathways. Non-PS samples are enriched for CD-1, PR, and CTA, the latter two associated with aggressive disease.
Methods: A 124-patient cohort with EMD (70 paraskeletal (PS) and 48 non-paraskeletal (non-PS)) from a single institution (Weill Cornell, WCM) were compared to a randomly selected non-EMD MM control group (232 patients). The MM Research Foundation (MMRF) CoMMpass registry was queried, and patients who developed non-PS EMD (184 patients) at any point were compared to non-EMD group (957 patients). Baseline characteristics and clinical outcomes were compared. Copy number alterations, structural variants, point mutations, differential expression analysis (DEA) and mutational signature were compared in the MMRF cohort from the sample at diagnosis. Analysis of Whole exome and RNA sequencing of 8 matched bone marrow-EMD biopsies is currently underway and will be available at the meeting.
Results: EMD is associated with lower M protein (p = 0.02) and higher hemoglobin (p < 0.01) at diagnosis in the MMRF. Lower OS (WCM: HR 3.4, CI 1.5-7.9 p < 0.01, MMRF: HR 1.5, CI 1.2-1.9, p = 0.018) and PFS (MMRF: HR 1.51, 95CI (1.23 - 1.87), p < 0.01) were seen in non-PS EMD after adjusting for ASCT use, presence of anemia, LDH, ISS, and high-risk cytogenetics. The use of ASCT, maintenance, and triplet induction led to improved outcomes, but the effect of EMD was not abrogated. Landmark analysis was performed in the MMRF for ASCT and maintenance with similar results.
Non-PS EMD was associated with higher rates of del17p (WCM 29% vs 14%, p 0.02), TP53 mutations (MMRF 9.6% vs 4.4%, p 0.02) and biallelic TP53 inactivation (MMRF 7.3% vs 2.9%, p 0.01), gain 1q (MMRF 44% vs 37%, WCM 47% vs 27%, p 0.01), del13q (WCM 53% vs 33%, p 0.02), Amp 8q24 (MYC, MMRF 27% vs 15%, p < 0.01) and del18q (MMRF 23% vs 14%, p < 0.01) when compared to non-EMD cases. There were no differences in mutations in top 25 recurrent genes. DEA and GSEA showed enrichment of the MYC target, E2F, G2M checkpoint pathways, and of the CD-1 (CCND1), CTA (cancer testis antigen), and PR (proliferative) myeloma subgroups, while there was lower expression of the focal adhesion molecules (FAC) pathway, MS, MF, and LB myeloma subgroups non-EMD samples. There were no differences in tumor mutation burden or selected COSMIC signature frequency between EMD and non-EMD samples.
Conclusions: Non-PS EMD is associated with worse clinical outcomes, with higher incidence of known high-risk molecular alterations (del17p, gain1q), in addition to other not previously identified such as amp8q24 (MYC). This correlates with enrichment for MYC and lower expression of FAC pathways. Non-PS samples are enriched for CD-1, PR, and CTA, the latter two associated with aggressive disease.
