Treatment of Newly Diagnosed Myeloma - Transplant Eligible
Poster Session 1
P-156: OUTCOMES OF A BORTEZOMIB-BASED INDUCTION REGIMEN (SEQUENTIAL OR UPFRONT TRIPLE ASSOCIATION WITH LENALIDOMIDE) IN TRANPLANT-ELIGIBLE PATIENTS WITH NEWLY DIAGNOSED MULTIPLE MYELOMA
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Joana Vieira, MD (she/her/hers)
Hematologist
Hospital Santa Maria, CHULN, Portugal
Introduction: The association of lenalidomide to bortezomib and dexamethasone (VRd) as induction therapy (IT) in newly diagnosed multiple myeloma (NDMM) patients (pts) eligible for autologous stem-cell transplantation (ASCT) has demonstrated excellent response rates and survival outcomes with manageable toxicities. Urgent treatment is often required in this setting and lenalidomide may not be immediately available for upfront use.
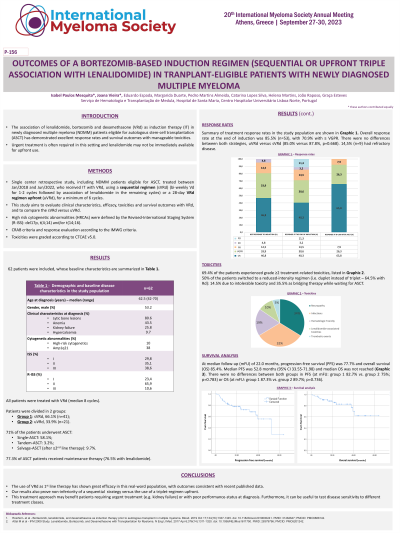
Methods: Single center retrospective study, including NDMM pts treated between Jan/2018-Jun/2022, who received IT with VRd, using a sequential regimen (sVRd) (bi-weekly Vd for 1-2 cycles followed by association of lenalidomide in the remaining cycles) or a 28-day VRd regimen upfront (uVRd), for 6 cycles. This study aims to evaluate clinical characteristics, efficacy, toxicities and survival outcomes with VRd and to compare the sVRd versus uVRd. High risk cytogenetic abnormalities (HRCAs) defined by the Revised-International Staging System (R-ISS): del17p, t(4;14) and/or t(14;16). CRAB criteria and response evaluation according to the IMWG criteria. Toxicities graded according to CTCAE v5.0.
Results: 62 pts; median age of 62.5 years (range 42-70); 53.2% male. Clinical characteristics at diagnosis: 80.6% lytic bone lesions, 43.5% anemia, 25.8% kidney failure and 9.7% hypercalcemia. 10% had HRCAs and 38% amp1q21 (FISH available in 79%). ISS stage III present in 37.3% and R-ISS stage III in 10.6%. All pts were treated with VRd (median 8 cycles), of which 66.1% (n=41) received sVRd (group 1) and 32.3% (n=20) received uVRd (group 2). 58.1% underwent single ASCT, 3.2% tandem ASCT and 9.7% salvage-ASCT (after ≥2nd line therapy). 77.3% of ASCT pts received maintenance therapy (76.5% including lenalidomide). 69.4% experienced grade ≥2 treatment-related toxicities: 32.3% peripheral neuropathy, 30.6% infection, 17.7% hematologic toxicity, 9.7% lenalidomide-related rash and 4.8% thrombotic events. Overall response rate at the end of IT was 85.5% (complete response 40.3%; very good partial response 30.6%; partial response [PR] 14.5%), with no differences between groups. 14.5% of the pts had treatment failure (< PR). At median follow-up (MFU) of 22.0 months (mo), progression-free survival (PFS) was 77.7% and overall survival (OS) 85.4%. Median PFS was 52.8 mo (95% CI 33.55-71.98) and median OS was not reached. There were no differences between groups in PFS (at MFU: gr1 82.7% vs. gr2 75%; p=0.783) or OS (at MFU: gr1 87.3% vs. gr2 89.7%; p=0.736).
Conclusions: The use of VRd as 1st line therapy has shown great efficacy in this real-word population, with outcomes consistent with recent published data. Our results also prove non-inferiority of a sequential strategy versus the use of a triplet-regimen upfront. This treatment approach may benefit pts requiring urgent treatment (e.g. kidney failure) or with poor performance-status at diagnosis. Furthermore, it can be useful to test disease sensitivity to different treatment classes.
Methods: Single center retrospective study, including NDMM pts treated between Jan/2018-Jun/2022, who received IT with VRd, using a sequential regimen (sVRd) (bi-weekly Vd for 1-2 cycles followed by association of lenalidomide in the remaining cycles) or a 28-day VRd regimen upfront (uVRd), for 6 cycles. This study aims to evaluate clinical characteristics, efficacy, toxicities and survival outcomes with VRd and to compare the sVRd versus uVRd. High risk cytogenetic abnormalities (HRCAs) defined by the Revised-International Staging System (R-ISS): del17p, t(4;14) and/or t(14;16). CRAB criteria and response evaluation according to the IMWG criteria. Toxicities graded according to CTCAE v5.0.
Results: 62 pts; median age of 62.5 years (range 42-70); 53.2% male. Clinical characteristics at diagnosis: 80.6% lytic bone lesions, 43.5% anemia, 25.8% kidney failure and 9.7% hypercalcemia. 10% had HRCAs and 38% amp1q21 (FISH available in 79%). ISS stage III present in 37.3% and R-ISS stage III in 10.6%. All pts were treated with VRd (median 8 cycles), of which 66.1% (n=41) received sVRd (group 1) and 32.3% (n=20) received uVRd (group 2). 58.1% underwent single ASCT, 3.2% tandem ASCT and 9.7% salvage-ASCT (after ≥2nd line therapy). 77.3% of ASCT pts received maintenance therapy (76.5% including lenalidomide). 69.4% experienced grade ≥2 treatment-related toxicities: 32.3% peripheral neuropathy, 30.6% infection, 17.7% hematologic toxicity, 9.7% lenalidomide-related rash and 4.8% thrombotic events. Overall response rate at the end of IT was 85.5% (complete response 40.3%; very good partial response 30.6%; partial response [PR] 14.5%), with no differences between groups. 14.5% of the pts had treatment failure (< PR). At median follow-up (MFU) of 22.0 months (mo), progression-free survival (PFS) was 77.7% and overall survival (OS) 85.4%. Median PFS was 52.8 mo (95% CI 33.55-71.98) and median OS was not reached. There were no differences between groups in PFS (at MFU: gr1 82.7% vs. gr2 75%; p=0.783) or OS (at MFU: gr1 87.3% vs. gr2 89.7%; p=0.736).
Conclusions: The use of VRd as 1st line therapy has shown great efficacy in this real-word population, with outcomes consistent with recent published data. Our results also prove non-inferiority of a sequential strategy versus the use of a triplet-regimen upfront. This treatment approach may benefit pts requiring urgent treatment (e.g. kidney failure) or with poor performance-status at diagnosis. Furthermore, it can be useful to test disease sensitivity to different treatment classes.
