Nursing Symposium
Poster Session 1
NSP-03: Practical Management of Patients With Relapsed/Refractory Multiple Myeloma Receiving Talquetamab, a GPRC5D×CD3 Bispecific Antibody: Experience in MonumenTAL-1
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Donna Catamero, ANP-BC, OCN, CCRC
Associate Director, Myeloma Translational Research
Mount Sinai Health System, New York, NY, USA, United States
Introduction: Talquetamab (tal) is a T-cell redirecting bispecific antibody targeting a novel antigen, G protein–coupled receptor family C group 5 member D (GPRC5D). Tal has shown overall response rates of >71% in patients with relapsed/refractory multiple myeloma (RRMM) in the MonumenTAL-1 study. Adverse events (AEs) reported with tal include those associated with T-cell redirection therapies as well as GPRC5D-related AEs. Here we provide guidance for administering tal and strategies for monitoring and managing AEs based on our experience in the MonumenTAL-1 study.
Methods: MonumenTAL-1 (NCT03399799/NCT04634552) is an open-label, single-arm, phase 1/2 study of patients with RRMM evaluating the recommended phase 2 doses of subcutaneous tal at 0.4 mg/kg weekly and 0.8 mg/kg every other week.
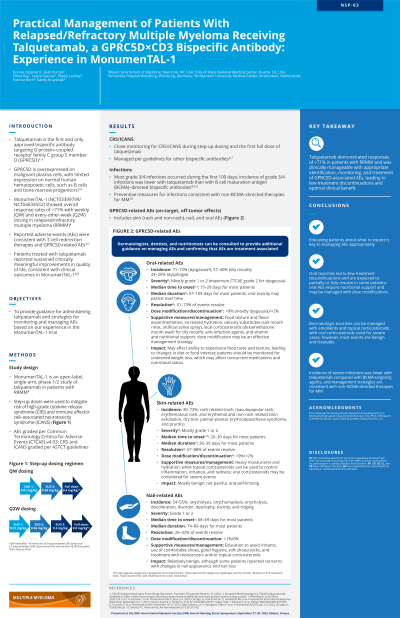
Results: Administration of tal includes initial “step-up” doses prior to the first full dose to mitigate risk of high-grade cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS). Similar to other bispecifics, these AEs appear early with tal and are generally mild to moderate. Patients should be premedicated appropriately and monitored closely for CRS/ICANS during step-up dosing and the first full dose. Infections are a common complication of MM; patients should be screened for infections before starting tal, receive prophylaxis as needed, and be monitored throughout treatment for infections. GPRC5D-related AEs, including dermatologic and oral toxicities, also tend to appear early, after the first few doses of tal. Dermatologic AEs (incidence ~30‒73%), including rash and skin peeling, are relatively benign, not painful, self-limiting, and manageable with emollients; nail AEs (incidence ~54‒63%), including nail thinning and loss, are mostly aesthetic but take time to resolve. Oral AEs (incidence ~71‒77%), including dysphagia (difficulty swallowing), dry mouth, and taste changes, tend to have longer duration and can affect patients’ quality of life; patients generally experience taste alteration with dry mouth that may lead to difficulty swallowing, which in turn can lead to weight loss. Supportive measures may be utilized (eg, NaCl mouth rinse, artificial saliva spray, diet modification) but oral AEs are most successfully managed with dose modification. A multidisciplinary team, including dermatologists, dentists, and nutritionists, can be consulted to provide additional guidance on managing GPRC5D-associated AEs. Educating patients about what to expect and ensuring they report symptoms promptly is also key to managing AEs appropriately. In general, patients respond well to treatment, and GPRC5D-associated AEs improve over time, becoming more tolerable; notable reduction in AEs is seen with dose modification.
Conclusions: Tal demonstrates responses in >71% of patients with RRMM, with a safety profile that can be clinically managed with appropriate identification, monitoring, and treatment to ensure patients receive optimal benefit of tal.
Methods: MonumenTAL-1 (NCT03399799/NCT04634552) is an open-label, single-arm, phase 1/2 study of patients with RRMM evaluating the recommended phase 2 doses of subcutaneous tal at 0.4 mg/kg weekly and 0.8 mg/kg every other week.
Results: Administration of tal includes initial “step-up” doses prior to the first full dose to mitigate risk of high-grade cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS). Similar to other bispecifics, these AEs appear early with tal and are generally mild to moderate. Patients should be premedicated appropriately and monitored closely for CRS/ICANS during step-up dosing and the first full dose. Infections are a common complication of MM; patients should be screened for infections before starting tal, receive prophylaxis as needed, and be monitored throughout treatment for infections. GPRC5D-related AEs, including dermatologic and oral toxicities, also tend to appear early, after the first few doses of tal. Dermatologic AEs (incidence ~30‒73%), including rash and skin peeling, are relatively benign, not painful, self-limiting, and manageable with emollients; nail AEs (incidence ~54‒63%), including nail thinning and loss, are mostly aesthetic but take time to resolve. Oral AEs (incidence ~71‒77%), including dysphagia (difficulty swallowing), dry mouth, and taste changes, tend to have longer duration and can affect patients’ quality of life; patients generally experience taste alteration with dry mouth that may lead to difficulty swallowing, which in turn can lead to weight loss. Supportive measures may be utilized (eg, NaCl mouth rinse, artificial saliva spray, diet modification) but oral AEs are most successfully managed with dose modification. A multidisciplinary team, including dermatologists, dentists, and nutritionists, can be consulted to provide additional guidance on managing GPRC5D-associated AEs. Educating patients about what to expect and ensuring they report symptoms promptly is also key to managing AEs appropriately. In general, patients respond well to treatment, and GPRC5D-associated AEs improve over time, becoming more tolerable; notable reduction in AEs is seen with dose modification.
Conclusions: Tal demonstrates responses in >71% of patients with RRMM, with a safety profile that can be clinically managed with appropriate identification, monitoring, and treatment to ensure patients receive optimal benefit of tal.
