Cellular and T cell engager Immunotherapy
Poster Session 1
P-007: Prognostic Impact of Corticosteroid and Tocilizumab Use on the Efficacy of Chimeric Antigen Receptor T-cell Therapy for Relapsed/Refractory Multiple Myeloma
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Bruno A. Costa, MD (he/him/his)
Medicine Resident
Mount Sinai Morningside and West, Icahn School of Medicine at Mount Sinai
New York, New York, United States
Introduction: Chimeric antigen receptor T-cell (CAR-T) therapy targeting B-cell maturation antigen (BCMA) or G protein-coupled receptor, class C, group 5, member D (GPRC5D) has shown unprecedented efficacy in patients (pts) with relapsed/refractory multiple myeloma (RRMM). Immune-related adverse events (irAEs) such as cytokine release syndrome (CRS) and neurotoxicity may occur early in treatment. Whilst immune-suppressive agents such as tocilizumab (TCZ) and corticosteroids (CS) are used to manage irAEs, a potential concern is a negative effect on CAR-T efficacy and survival outcomes. Here, we evaluated the prognostic impact of TCZ and CS use within 30 days of CAR-T infusion.
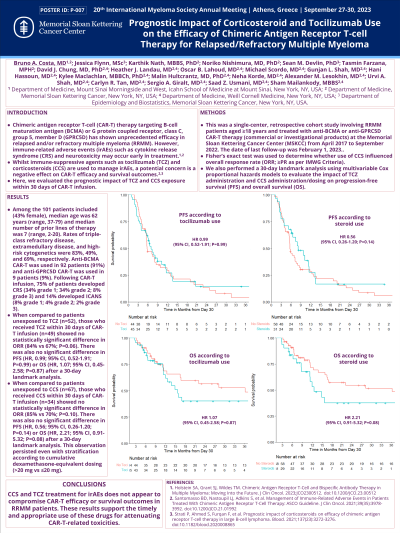
Methods: This was a single-center, retrospective cohort study involving RRMM pts aged ≥18 years and treated with commercial/investigational anti-BCMA or anti-GPRC5D CAR-T therapy from April 2017 to September 2022. Fisher’s exact test was used to determine whether CS use influenced the overall response rate (ORR; ≥PR as per IMWG Criteria). We also performed a 30-day landmark analysis using multivariable Cox proportional hazards models to evaluate the impact of TCZ administration and CS administration/dosing on progression-free survival (PFS) and overall survival (OS).
Results: Among the 102 pts included (46% female), the median age was 62 years (range, 37-79) and median number of prior lines of therapy was 6 (range, 2-20). Triple-class refractoriness (TCR), extramedullary disease (EMD), and high-risk cytogenetics were present in 83%, 49%, and 70% of pts, respectively. Anti-BCMA CAR-T was used in 93 pts (91%), and anti-GPRC5D CAR-T in 9 pts (9%). After CAR-T infusion, 77% of pts developed CRS (35% grade 1; 34% grade 2; 8% grade 3) and 14% developed neurotoxicity (8% grade 1; 4% grade 2; 2% grade 3). A total of 42 pts (41%) and 29 pts (28%) received TCZ and CS within 30 days post-infusion, respectively. No significant difference in ORR was observed between pts who received CS and those that did not (66% vs 83%; P=0.089). Following a 30-day landmark analysis, both PFS and OS were significantly inferior in pts with EMD with hazard ratio (HR) of 1.86 (95% confidence interval [CI], 1.05-3.29; P=0.034) and 3.88 (95% CI, 1.71-8.76; P< 0.001), respectively, after adjusting for covariates. There was no significant difference in either PFS (HR, 0.9; 95% CI, 0.43-1.89; P=0.78) or OS (HR, 1.37; 95% CI, 0.49-3.80; P=0.54) in pts who received CS within 30 days of CAR-T infusion. This was maintained even after stratification according to total dexamethasone-equivalent dosing (>20 mg vs ≤20 mg). Similarly, there was no significant difference in either PFS (HR, 1.06; 95% CI, 0.55-2.04; P=0.87) or OS (HR, 1.03; 95% CI, 0.40-2.68; P=0.95) in pts who received TCZ versus those that did not.
Conclusions: CS and TCZ treatment for irAEs does not appear to compromise CAR-T efficacy or survival outcomes in RRMM pts. These results support the timely and appropriate use of these drugs for attenuating CAR-T-related toxicities.
Methods: This was a single-center, retrospective cohort study involving RRMM pts aged ≥18 years and treated with commercial/investigational anti-BCMA or anti-GPRC5D CAR-T therapy from April 2017 to September 2022. Fisher’s exact test was used to determine whether CS use influenced the overall response rate (ORR; ≥PR as per IMWG Criteria). We also performed a 30-day landmark analysis using multivariable Cox proportional hazards models to evaluate the impact of TCZ administration and CS administration/dosing on progression-free survival (PFS) and overall survival (OS).
Results: Among the 102 pts included (46% female), the median age was 62 years (range, 37-79) and median number of prior lines of therapy was 6 (range, 2-20). Triple-class refractoriness (TCR), extramedullary disease (EMD), and high-risk cytogenetics were present in 83%, 49%, and 70% of pts, respectively. Anti-BCMA CAR-T was used in 93 pts (91%), and anti-GPRC5D CAR-T in 9 pts (9%). After CAR-T infusion, 77% of pts developed CRS (35% grade 1; 34% grade 2; 8% grade 3) and 14% developed neurotoxicity (8% grade 1; 4% grade 2; 2% grade 3). A total of 42 pts (41%) and 29 pts (28%) received TCZ and CS within 30 days post-infusion, respectively. No significant difference in ORR was observed between pts who received CS and those that did not (66% vs 83%; P=0.089). Following a 30-day landmark analysis, both PFS and OS were significantly inferior in pts with EMD with hazard ratio (HR) of 1.86 (95% confidence interval [CI], 1.05-3.29; P=0.034) and 3.88 (95% CI, 1.71-8.76; P< 0.001), respectively, after adjusting for covariates. There was no significant difference in either PFS (HR, 0.9; 95% CI, 0.43-1.89; P=0.78) or OS (HR, 1.37; 95% CI, 0.49-3.80; P=0.54) in pts who received CS within 30 days of CAR-T infusion. This was maintained even after stratification according to total dexamethasone-equivalent dosing (>20 mg vs ≤20 mg). Similarly, there was no significant difference in either PFS (HR, 1.06; 95% CI, 0.55-2.04; P=0.87) or OS (HR, 1.03; 95% CI, 0.40-2.68; P=0.95) in pts who received TCZ versus those that did not.
Conclusions: CS and TCZ treatment for irAEs does not appear to compromise CAR-T efficacy or survival outcomes in RRMM pts. These results support the timely and appropriate use of these drugs for attenuating CAR-T-related toxicities.
