Other plasma cell disorders
Poster Session 3
P-421: Reference interval of free light chain ratio for patients in chronic hemodialysis
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Pablo Bustamante, MD
Internal Medicine Trainee
Hospital del Salvador, Chile
Introduction: In patients with chronic kidney disease (CKD), the concentration of serum free light chains (FLC) increases proportionally to the degree of reduction in glomerular filtration rate (GFR). The currently used reference range of the FLC ratio (FLCr) Kappa/Lambda (K/L) in patients with CKD is between 0.37 and 3.1. Nevertheless, the normal range of FLCr in patients in hemodialysis (HD) is unclear. Recently, Long et al reported new FLCr ranges according to CKD stage, based on estimated GFR. However, this study considered only a few patients on HD.
Methods: This is an observational and analytical cohort study. Patients on HD from a single HD center were included. They had more than 3 months of permanence on conventional HD, 3 times a week, with a high-flux membrane (Helixone®). K and L FLC determinations were performed using the Freelite® assay according to the Laboratory's instructions (Binding Site, Birmingham, UK). We determined K and L values, and the K/L ratio. These results were correlated with age and residual kidney function (RKF), defined as residual diuresis ≥250mL/day. 95% reference intervals values were calculated according to the recommendations of The Clinical and Laboratory Standards Institute (CLSI EP28-A3c). Atypical data (outliers) were evaluated with Tukey's test, and not removed from the analysis. Normality was evaluated with the D'agostino Pearson test. For monoclonal gammopathy (MG) detection, we performed capillary sPEP and FLC to all patients. In patients with monoclonal spike, hypogammaglobulinemia or altered FLCr, immunosubtraction (Sebia) was also performed. Analysis was made with Software Medcalc v20.104 and SPSS. The protocol was approved by the local Institutional Review Board.
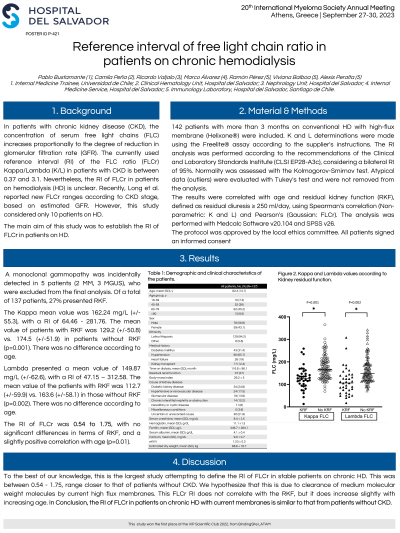
Results: A total of 138 patients were studied, since 5 patients with MG incidentally detected were excluded (2 MM, 3 MGUS).
K showed a non-parametric distribution, with a mean of 162.24 mg/L (64.46 - 281.76 mg/L). L also showed a non-parametric distribution, with a mean of 149.87mg/L (47.15 - 312.58 mg/L). The reference range of FLCr showed a parametric distribution of 0.54 to 1.75.
Both K and L increases with age until the 9th decade when they tend to decrease.
Twenty-four percent of the patients still presented RKF. The results in both groups (with vs without RKF, respectively) were for K 128.69 +/- 51.4 mg/L vs 174.48 +/- 52.19 mg/L (p < 0.01); For Lambda 111.30 +/- 60.11 mg/L vs 163.82 +/- 58.32mg/L (p < 0.01). Regarding the K/L ratio, in patients with RKF was 1.24 +/- 0.32, while in patients without RKF was 1.12 +/- 0.30 (p < 0.04).
Conclusions: To our knowledge, this is the largest study that attempts to define the reference interval of FLCr in stable patients on chronic HD. The K/L ratio in this population was 0.54 - 1.75, closer to that of patients without CKD. We hypothesize that this is due to the clearance of middle molecules by the high-flux membranes. The ratio and FLC levels are influenced by the RKF.
Methods: This is an observational and analytical cohort study. Patients on HD from a single HD center were included. They had more than 3 months of permanence on conventional HD, 3 times a week, with a high-flux membrane (Helixone®). K and L FLC determinations were performed using the Freelite® assay according to the Laboratory's instructions (Binding Site, Birmingham, UK). We determined K and L values, and the K/L ratio. These results were correlated with age and residual kidney function (RKF), defined as residual diuresis ≥250mL/day. 95% reference intervals values were calculated according to the recommendations of The Clinical and Laboratory Standards Institute (CLSI EP28-A3c). Atypical data (outliers) were evaluated with Tukey's test, and not removed from the analysis. Normality was evaluated with the D'agostino Pearson test. For monoclonal gammopathy (MG) detection, we performed capillary sPEP and FLC to all patients. In patients with monoclonal spike, hypogammaglobulinemia or altered FLCr, immunosubtraction (Sebia) was also performed. Analysis was made with Software Medcalc v20.104 and SPSS. The protocol was approved by the local Institutional Review Board.
Results: A total of 138 patients were studied, since 5 patients with MG incidentally detected were excluded (2 MM, 3 MGUS).
K showed a non-parametric distribution, with a mean of 162.24 mg/L (64.46 - 281.76 mg/L). L also showed a non-parametric distribution, with a mean of 149.87mg/L (47.15 - 312.58 mg/L). The reference range of FLCr showed a parametric distribution of 0.54 to 1.75.
Both K and L increases with age until the 9th decade when they tend to decrease.
Twenty-four percent of the patients still presented RKF. The results in both groups (with vs without RKF, respectively) were for K 128.69 +/- 51.4 mg/L vs 174.48 +/- 52.19 mg/L (p < 0.01); For Lambda 111.30 +/- 60.11 mg/L vs 163.82 +/- 58.32mg/L (p < 0.01). Regarding the K/L ratio, in patients with RKF was 1.24 +/- 0.32, while in patients without RKF was 1.12 +/- 0.30 (p < 0.04).
Conclusions: To our knowledge, this is the largest study that attempts to define the reference interval of FLCr in stable patients on chronic HD. The K/L ratio in this population was 0.54 - 1.75, closer to that of patients without CKD. We hypothesize that this is due to the clearance of middle molecules by the high-flux membranes. The ratio and FLC levels are influenced by the RKF.
