Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-328: Talquetamab vs Real-World Physician’s Choice of Therapy (RWPC): Comparative Efficacy in Patients (pts) With Triple-Class Exposed (TCE) Relapsed/Refractory Multiple Myeloma (RRMM)
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST
- JY
Jing Christine Ye, MD, MSc
Associate Professor
UT MD Anderson Cancer Center, TX, USA (currently); University of Michigan, Rogel Cancer Center, Ann Arbor, MI, USA (during study), United States
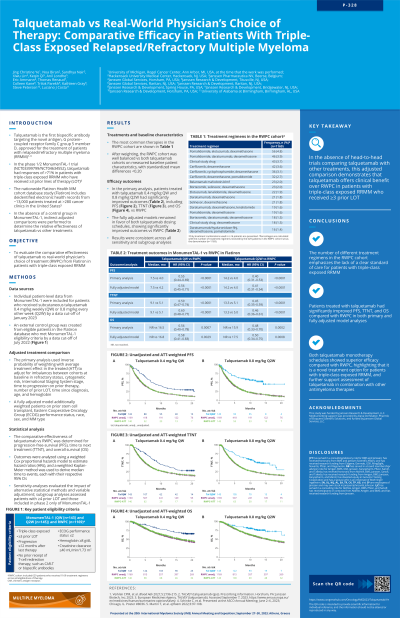
Introduction: In MonumenTAL-1 (NCT03399799/NCT04634552), talquetamab, a G protein–coupled receptor family C group 5 member D × CD3 bispecific antibody, had an overall response rate of >71% in TCE pts with RRMM who received ≥3 prior lines of therapy (LOT). To assess the relative effectiveness of both recommended phase 2 doses (RP2Ds) of talquetamab vs RWPC, adjusted comparisons were performed using individual patient-level data from MonumenTAL-1 and the Flatiron Health MM cohort database study (Flatiron).
Methods: An external control arm for MonumenTAL-1 was created from eligible pts in the Flatiron database (data cut-off [DCO] Aug 2022) who met key MonumenTAL-1 eligibility criteria (N=629 with 1169 eligible LOT). Individual patient-level data from MonumenTAL-1 were included for pts who received subcutaneous (SC) talquetamab 0.4 mg/kg weekly (QW; n=143) and SC talquetamab 0.8 mg/kg every other week (Q2W; n=145) utilizing a Jan 17, 2023 DCO. In the base model, baseline characteristics of prognostic variables (refractory status, cytogenetic risk, International Staging System stage, time to disease progression on last LOT, number of prior LOT, time since diagnosis, age, and hemoglobin) were adjusted using inverse probability of treatment weighting. The full model was adjusted for the base model variables as well as prior stem cell transplant, ECOG performance status, race, sex, and MM type. Efficacy outcomes were progression-free survival (PFS), time to next treatment (TTNT), and overall survival (OS). A weighted Cox proportional hazards model was used to derive hazard ratios (HRs) and 95% CIs for time-to-event endpoints; a weighted Kaplan-Meier method was used to derive median time-to-events. Sensitivity analyses assessed the impact of alternative statistical methods and variable adjustment.
Results: After weighting, baseline characteristics were balanced across cohorts, with standardized mean differences < 0.2. In the base case analysis, compared with RWPC, pts treated with both RP2Ds of talquetamab had significantly improved PFS (QW: 7.5 vs 4.0 months [mo], HR=0.55, 95% CI 0.44–0.69, P< 0.0001; Q2W: 14.2 vs 4.0 mo, HR=0.40, 95% CI 0.31–0.53, P< 0.0001), TTNT (QW: 9.1 vs 5.1 mo, HR=0.59, 95% CI 0.47–0.74, P< 0.0001; Q2W: 13.3 vs 5.1 mo, HR=0.45, 95% CI 0.35–0.59, P< 0.0001), and OS (QW: not reached vs 16.5 mo, HR=0.56, 95% CI 0.40–0.78, P=0.0007; Q2W: not reached vs 15.9 mo, HR=0.48, 95% CI 0.33–0.70, P=0.0002). The fully adjusted models and sensitivity analyses remained in favor of talquetamab for both RP2Ds, consistent with the base case.
Conclusions: Both RP2Ds of talquetamab significantly improved effectiveness vs RWPC across all outcomes. These data highlight the potential of talquetamab as an effective treatment option in pts with TCE RRMM and support the rationale of planned prospective trials to compare talquetamab with standard of care regimens in this patient population.
Methods: An external control arm for MonumenTAL-1 was created from eligible pts in the Flatiron database (data cut-off [DCO] Aug 2022) who met key MonumenTAL-1 eligibility criteria (N=629 with 1169 eligible LOT). Individual patient-level data from MonumenTAL-1 were included for pts who received subcutaneous (SC) talquetamab 0.4 mg/kg weekly (QW; n=143) and SC talquetamab 0.8 mg/kg every other week (Q2W; n=145) utilizing a Jan 17, 2023 DCO. In the base model, baseline characteristics of prognostic variables (refractory status, cytogenetic risk, International Staging System stage, time to disease progression on last LOT, number of prior LOT, time since diagnosis, age, and hemoglobin) were adjusted using inverse probability of treatment weighting. The full model was adjusted for the base model variables as well as prior stem cell transplant, ECOG performance status, race, sex, and MM type. Efficacy outcomes were progression-free survival (PFS), time to next treatment (TTNT), and overall survival (OS). A weighted Cox proportional hazards model was used to derive hazard ratios (HRs) and 95% CIs for time-to-event endpoints; a weighted Kaplan-Meier method was used to derive median time-to-events. Sensitivity analyses assessed the impact of alternative statistical methods and variable adjustment.
Results: After weighting, baseline characteristics were balanced across cohorts, with standardized mean differences < 0.2. In the base case analysis, compared with RWPC, pts treated with both RP2Ds of talquetamab had significantly improved PFS (QW: 7.5 vs 4.0 months [mo], HR=0.55, 95% CI 0.44–0.69, P< 0.0001; Q2W: 14.2 vs 4.0 mo, HR=0.40, 95% CI 0.31–0.53, P< 0.0001), TTNT (QW: 9.1 vs 5.1 mo, HR=0.59, 95% CI 0.47–0.74, P< 0.0001; Q2W: 13.3 vs 5.1 mo, HR=0.45, 95% CI 0.35–0.59, P< 0.0001), and OS (QW: not reached vs 16.5 mo, HR=0.56, 95% CI 0.40–0.78, P=0.0007; Q2W: not reached vs 15.9 mo, HR=0.48, 95% CI 0.33–0.70, P=0.0002). The fully adjusted models and sensitivity analyses remained in favor of talquetamab for both RP2Ds, consistent with the base case.
Conclusions: Both RP2Ds of talquetamab significantly improved effectiveness vs RWPC across all outcomes. These data highlight the potential of talquetamab as an effective treatment option in pts with TCE RRMM and support the rationale of planned prospective trials to compare talquetamab with standard of care regimens in this patient population.
