Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-250: THE RELATIONSHIP OF EXTRAMEDULLARY DISEASE AND HIGH-RISK CYTOGENETICS ON REAL-WORLD OUTCOMES AMONG PATIENTS WITH TRIPLE-CLASS EXPOSED MULTIPLE MYELOMA
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Marco DiBonaventura, PhD (he/him/his)
Senior Director, Value & Evidence Team Lead, Hematology & Biosimilars
Pfizer Inc
New York, New York, United States
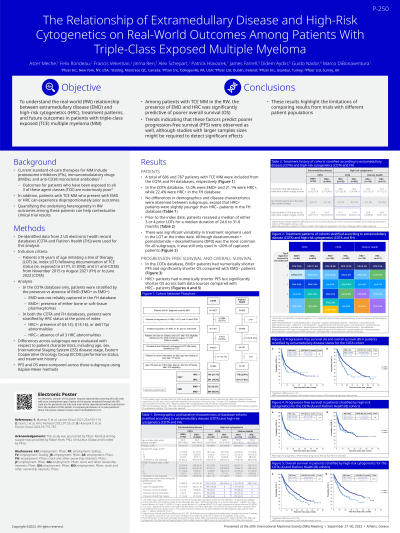
Introduction: Triple-class exposed (TCE) multiple myeloma (MM) patients who present with extramedullary disease (EMD) or high-risk cytogenetics can experience disproportionately poor outcomes. The current study sought to examine the real-world relationship between these disease attributes, treatment patterns, and future outcomes.
Methods: Using two US electronic health record databases (COTA and Flatiron Health), MM patients ≥18 years who initiated a subsequent therapy (ie, index regimen) after becoming TCE (ie, exposed to ≥1 PI, ≥1 IMiD, ≥1 anti-CD38) between November 2015 and June 2022 (COTA)/August 2021 (Flatiron) were included. Within the COTA database, patients were stratified by the presence versus absence of EMD (EMD+ vs. EMD-) and high-risk cytogenetics (HRC) (defined based on the presence of t(4:14), t(14:16), or del17p [ie, HRC+] or the absence of all three [HRC-] at the point of index). Because EMD was not reliably captured in the Flatiron Health database, only HRC comparisons were made in that data source. Differences across subgroups were evaluated with respect to patient characteristics (age, sex, ISS, ECOG), and treatment history. Progression-free survival (PFS) and overall survival (OS) were compared across these subgroups using the Kaplan-Meier method.
Results: Of the N=686 TCE MM patients included from the COTA database, 12.0% were EMD+ and 21.1% were HRC+. No demographic or disease characteristic differences were observed between subgroups. There was significant variability in treatment regimens with no regimen occurring in more than 13% of either subgroup. Daratumumab+pomalidomide+dexamethasone (DPd) was the most common for all subgroups (EMD+: 9.8%; EMD-: 11.8%; HRC+:13.8%; HRC-: 10.9%). Of the N=787 TCE MM patients included from the Flatiron database, 22.4% were HRC+. HRC+ patients were slightly younger (65.2 vs. 68.3 years, p<.05) but otherwise similar with respect to demographics and disease characteristics compared with HRC-. DPd was also the most common regimen for both HRC+ (6.3%) and HRC- (9.5%). In the COTA database, EMD+ patients reported directionally shorter PFS (median: 4.7 vs 9.9 months, log-rank p=.08) and significantly shorter OS compared with EMD- (median: 11.6 vs. 24.0 months, log-rank p<.05). HRC+ patients had directionally shorter PFS (COTA: median 8.3 vs. 9.5 months, log-rank p=.17; Flatiron: median 7.0 vs. 12.1, p=.09) but significantly shorter OS (COTA: 13.7 vs. 23.9 months, log-rank p<.05; Flatiron: 11.8 vs. 25.2 months, log-rank p<.05) across both data sources.
Conclusions: Among TCE MM patients in the real world, the presence of EMD and HRC was significantly predictive of poorer OS. Trends indicating that these factors predict poorer PFS were observed as well, though studies with larger samples sizes might be required to detect significant effects.
Methods: Using two US electronic health record databases (COTA and Flatiron Health), MM patients ≥18 years who initiated a subsequent therapy (ie, index regimen) after becoming TCE (ie, exposed to ≥1 PI, ≥1 IMiD, ≥1 anti-CD38) between November 2015 and June 2022 (COTA)/August 2021 (Flatiron) were included. Within the COTA database, patients were stratified by the presence versus absence of EMD (EMD+ vs. EMD-) and high-risk cytogenetics (HRC) (defined based on the presence of t(4:14), t(14:16), or del17p [ie, HRC+] or the absence of all three [HRC-] at the point of index). Because EMD was not reliably captured in the Flatiron Health database, only HRC comparisons were made in that data source. Differences across subgroups were evaluated with respect to patient characteristics (age, sex, ISS, ECOG), and treatment history. Progression-free survival (PFS) and overall survival (OS) were compared across these subgroups using the Kaplan-Meier method.
Results: Of the N=686 TCE MM patients included from the COTA database, 12.0% were EMD+ and 21.1% were HRC+. No demographic or disease characteristic differences were observed between subgroups. There was significant variability in treatment regimens with no regimen occurring in more than 13% of either subgroup. Daratumumab+pomalidomide+dexamethasone (DPd) was the most common for all subgroups (EMD+: 9.8%; EMD-: 11.8%; HRC+:13.8%; HRC-: 10.9%). Of the N=787 TCE MM patients included from the Flatiron database, 22.4% were HRC+. HRC+ patients were slightly younger (65.2 vs. 68.3 years, p<.05) but otherwise similar with respect to demographics and disease characteristics compared with HRC-. DPd was also the most common regimen for both HRC+ (6.3%) and HRC- (9.5%). In the COTA database, EMD+ patients reported directionally shorter PFS (median: 4.7 vs 9.9 months, log-rank p=.08) and significantly shorter OS compared with EMD- (median: 11.6 vs. 24.0 months, log-rank p<.05). HRC+ patients had directionally shorter PFS (COTA: median 8.3 vs. 9.5 months, log-rank p=.17; Flatiron: median 7.0 vs. 12.1, p=.09) but significantly shorter OS (COTA: 13.7 vs. 23.9 months, log-rank p<.05; Flatiron: 11.8 vs. 25.2 months, log-rank p<.05) across both data sources.
Conclusions: Among TCE MM patients in the real world, the presence of EMD and HRC was significantly predictive of poorer OS. Trends indicating that these factors predict poorer PFS were observed as well, though studies with larger samples sizes might be required to detect significant effects.
