Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-244: Teclistamab versus Belgian real-world clinical practice in triple-class exposed relapsed and refractory multiple myeloma patients using adjusted comparison.
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Michel Delforge, MD/Phd
Professor of Medicine
University of Leuven, Leuven, Belgium
Leuven, Belgium
Introduction: Triple-class exposed (TCE) relapsed and refractory multiple myeloma (RRMM) patients have a poor prognosis and limited treatment options. Teclistamab, a BCMA x CD3 bispecific antibody, is being studied in TCE RRMM patients in the single-arm phase 1/2 MajesTEC-1 trial. We assessed the relative effectiveness of teclistamab vs Belgian real-world clinical practice (RWCP) using individual patient data (IPD) from MajesTEC-1 and BELCOMM (Belgium Comparator study in Multiple Myeloma).
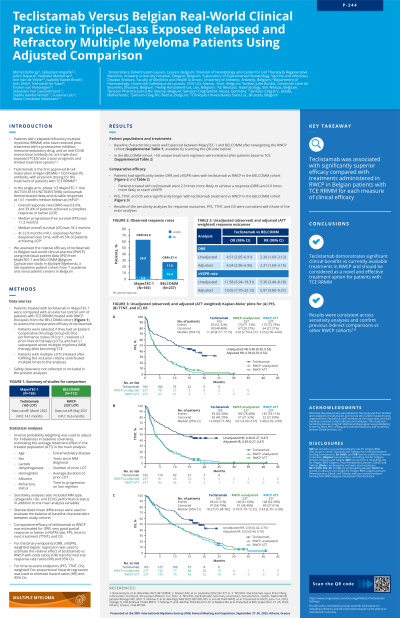
Methods: An external control arm for MajesTEC-1 was created from TCE RRMM patients treated with RWCP therapies from the BELCOMM cohort, a retrospective Belgian patient cohort. Patients with an ECOG score 0 or 1, who received ≥ 3 prior lines of therapy (LOTs), and at least 1 subsequent active MM therapy after becoming TCE, were selected. IPD were available for MajesTEC-1 patients (cut-off March 2022) and RWCP patients in the BELCOMM cohort (cut-off May 2021). Patients with multiple LOTs initiated after fulfilling the inclusion criteria contributed multiple times to the analyses. Inverse probability weighting (IPW) was used to adjust for imbalances in baseline covariates, estimating the average treatment effect in the treated population. Comparative effectiveness of teclistamab vs RWCP was estimated for overall response rate (ORR), very good partial response or better (≥VGPR) rate, progression-free survival (PFS), time to next treatment (TTNT) and overall survival (OS). For the binary endpoints (ORR and ≥VGPR), weighted logistic regression was used to estimate the relative effect of teclistamab vs RWCP with odds ratios (OR) transformed into response-rate ratios (RR) and 95% confidence intervals (CI). For time-to event endpoints (PFS, TTNT and OS) weighted Cox proportional hazards regression was used to estimate hazard ratios (HR) and 95% CIs.
Results: 165 patients (165 LOTs) from the MajesTEC-1 cohort and 112 patients (237 LOTs) from the BELCOMM cohort were included in the intention-to-treat (ITT) analyses. All adjusted comparative analyses demonstrated statistically significant results in favor of teclistamab across all endpoints. The RR for teclistamab vs RPWC for ORR and ≥VGPR were 2.31 [95% CI: 1.69, 3.15] and 5.97 [3.80, 9.37], respectively. Teclistamab patients were 2.3 and 6.0 times more likely to reach ORR and ≥VGPR, respectively. The HR for teclistamab vs RWPC were 0.39 [0.29, 0.52] for PFS, 0.35 [0.27, 0.47] for TTNT, and 0.55 [0.40, 0.76] for OS. Sensitivity analyses using multivariable logistic regression and Cox regression analysis were consistent with the main analyses.
Conclusions: Teclistamab was associated with significantly superior effectiveness compared with treatments administered in RWCP in Belgian TCE RRMM patients for each measure of clinical effectiveness. Results were consistent across sensitivity analyses and confirm previous indirect comparisons vs other RWPC cohorts. These findings highlight teclistamab's clinical benefit as a novel and effective treatment in TCE RRMM patients.
Methods: An external control arm for MajesTEC-1 was created from TCE RRMM patients treated with RWCP therapies from the BELCOMM cohort, a retrospective Belgian patient cohort. Patients with an ECOG score 0 or 1, who received ≥ 3 prior lines of therapy (LOTs), and at least 1 subsequent active MM therapy after becoming TCE, were selected. IPD were available for MajesTEC-1 patients (cut-off March 2022) and RWCP patients in the BELCOMM cohort (cut-off May 2021). Patients with multiple LOTs initiated after fulfilling the inclusion criteria contributed multiple times to the analyses. Inverse probability weighting (IPW) was used to adjust for imbalances in baseline covariates, estimating the average treatment effect in the treated population. Comparative effectiveness of teclistamab vs RWCP was estimated for overall response rate (ORR), very good partial response or better (≥VGPR) rate, progression-free survival (PFS), time to next treatment (TTNT) and overall survival (OS). For the binary endpoints (ORR and ≥VGPR), weighted logistic regression was used to estimate the relative effect of teclistamab vs RWCP with odds ratios (OR) transformed into response-rate ratios (RR) and 95% confidence intervals (CI). For time-to event endpoints (PFS, TTNT and OS) weighted Cox proportional hazards regression was used to estimate hazard ratios (HR) and 95% CIs.
Results: 165 patients (165 LOTs) from the MajesTEC-1 cohort and 112 patients (237 LOTs) from the BELCOMM cohort were included in the intention-to-treat (ITT) analyses. All adjusted comparative analyses demonstrated statistically significant results in favor of teclistamab across all endpoints. The RR for teclistamab vs RPWC for ORR and ≥VGPR were 2.31 [95% CI: 1.69, 3.15] and 5.97 [3.80, 9.37], respectively. Teclistamab patients were 2.3 and 6.0 times more likely to reach ORR and ≥VGPR, respectively. The HR for teclistamab vs RWPC were 0.39 [0.29, 0.52] for PFS, 0.35 [0.27, 0.47] for TTNT, and 0.55 [0.40, 0.76] for OS. Sensitivity analyses using multivariable logistic regression and Cox regression analysis were consistent with the main analyses.
Conclusions: Teclistamab was associated with significantly superior effectiveness compared with treatments administered in RWCP in Belgian TCE RRMM patients for each measure of clinical effectiveness. Results were consistent across sensitivity analyses and confirm previous indirect comparisons vs other RWPC cohorts. These findings highlight teclistamab's clinical benefit as a novel and effective treatment in TCE RRMM patients.
