Treatment of Relapsed/Refractory Myeloma
Poster Session 2
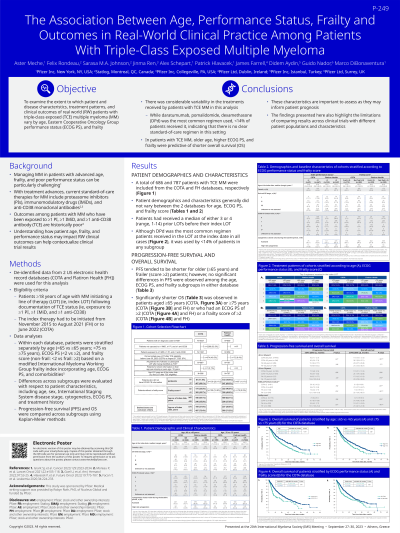
P-249: THE ASSOCIATION BETWEEN AGE, PERFORMANCE STATUS, FRAILTY AND OUTCOMES IN REAL-WORLD CLINICAL PRACTICE AMONG PATIENTS WITH TRIPLE-CLASS EXPOSED MULTIPLE MYELOMA
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Marco DiBonaventura, PhD (he/him/his)
Senior Director, Value & Evidence Team Lead, Hematology & Biosimilars
Pfizer Inc
New York, New York, United States
Introduction: Disease management in multiple myeloma (MM) among those with advanced age and poorer functioning can be particularly challenging (Grant et al 2023). The objective of the current study was to examine the extent to which patient outcomes vary by age, performance status based on the ECOG score, and frailty, based on a modified IMWG frailty index, among those who have already been exposed to at least 1 proteasome inhibitor, 1 immunomodulatory drug, and 1 anti-CD38 antibody (ie, triple-class exposed [TCE]).
Methods: Patients ≥18 years with MM who initiated a subsequent therapy (ie, index regimen) after becoming TCE were identified through two US electronic health record databases (COTA and Flatiron Health). In each database, patients were stratified by age ( < 65 vs ≥65; < 75 vs ≥75), ECOG score ( < 2 vs ≥2), and frailty score (non-frail: < 2 vs frail: ≥2) based on a modified IMWG frailty index incorporating age, ECOG, and comorbidities. Differences across subgroups were evaluated with respect to patient characteristics (age, sex, ISS, cytogenetics) and treatment history. Progression-free survival (PFS) and overall survival (OS) were compared across these subgroups using Kaplan-Meier methods.
Results: A total of N=686 TCE MM patients were included from the COTA database: 64.1% were ≥65 years (yrs), 27.6% were ≥75 yrs, 11.8% were ECOG≥2, and 25.5% were frail. Though median (m)PFS tended to be shorter for older and poorer functioning patients, PFS results were not statistically significantly different across all comparisons. However, patients ≥65 yrs had significantly shorter OS than patients < 65 yrs (mOS=17.6 vs 28.7 months, log-rank p<.05) and patients ≥75 yrs had significantly shorter OS than patients < 75 yrs (mOS=17.0 vs 24.1 months, log-rank p<.05). Similarly, ECOG≥2 and frail patients had significantly shorter (log-rank ps <.05) OS than ECOG < 2 and non-frail patients, respectively (mOS=8.1 vs 21.0 months; 12.7 vs 21.9 months). Results within the Flatiron database (N=787) were generally similar: 62.1% were ≥65 yrs, 28.8% were ≥75 yrs, 19.4% were ECOG≥2, and 40.9% were frail. PFS results were not statistically significantly different across all comparisons (log-rank p≥.05). As in the COTA database, patients ≥75 yrs had significantly shorter OS than patients < 75 yrs (mOS=17.5 vs 23.3 months, log-rank p<.05). Similarly, ECOG≥2 and frail patients had significantly shorter OS than ECOG < 2 and non-frail patients respectively (mOS=11.4 vs 25.0 months, log-rank p<.05; mOS=12.9 vs 27.4 months, log-rank p<.05).
Conclusions: Older age, higher ECOG score, and being frail were generally not significantly predictive of shorter PFS, but they were predictive of shorter OS.
Methods: Patients ≥18 years with MM who initiated a subsequent therapy (ie, index regimen) after becoming TCE were identified through two US electronic health record databases (COTA and Flatiron Health). In each database, patients were stratified by age ( < 65 vs ≥65; < 75 vs ≥75), ECOG score ( < 2 vs ≥2), and frailty score (non-frail: < 2 vs frail: ≥2) based on a modified IMWG frailty index incorporating age, ECOG, and comorbidities. Differences across subgroups were evaluated with respect to patient characteristics (age, sex, ISS, cytogenetics) and treatment history. Progression-free survival (PFS) and overall survival (OS) were compared across these subgroups using Kaplan-Meier methods.
Results: A total of N=686 TCE MM patients were included from the COTA database: 64.1% were ≥65 years (yrs), 27.6% were ≥75 yrs, 11.8% were ECOG≥2, and 25.5% were frail. Though median (m)PFS tended to be shorter for older and poorer functioning patients, PFS results were not statistically significantly different across all comparisons. However, patients ≥65 yrs had significantly shorter OS than patients < 65 yrs (mOS=17.6 vs 28.7 months, log-rank p<.05) and patients ≥75 yrs had significantly shorter OS than patients < 75 yrs (mOS=17.0 vs 24.1 months, log-rank p<.05). Similarly, ECOG≥2 and frail patients had significantly shorter (log-rank ps <.05) OS than ECOG < 2 and non-frail patients, respectively (mOS=8.1 vs 21.0 months; 12.7 vs 21.9 months). Results within the Flatiron database (N=787) were generally similar: 62.1% were ≥65 yrs, 28.8% were ≥75 yrs, 19.4% were ECOG≥2, and 40.9% were frail. PFS results were not statistically significantly different across all comparisons (log-rank p≥.05). As in the COTA database, patients ≥75 yrs had significantly shorter OS than patients < 75 yrs (mOS=17.5 vs 23.3 months, log-rank p<.05). Similarly, ECOG≥2 and frail patients had significantly shorter OS than ECOG < 2 and non-frail patients respectively (mOS=11.4 vs 25.0 months, log-rank p<.05; mOS=12.9 vs 27.4 months, log-rank p<.05).
Conclusions: Older age, higher ECOG score, and being frail were generally not significantly predictive of shorter PFS, but they were predictive of shorter OS.
