Treatment of Relapsed/Refractory Myeloma
Poster Session 2
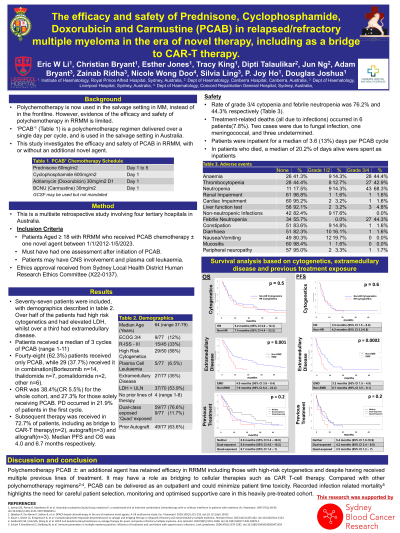
P-289: The efficacy and safety of Prednisone, Cyclophosphamide, Doxorubicin and Carmustine (PCAB) in relapsed/refractory multiple myeloma in the era of novel therapy, including as a bridge to CAR-T therapy.
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST
Eric W. Li, MBBS, BPharm(Hons), FRACP, FRCPA
Haematology Fellow
Royal Prince Alfred Hospital
Malabar, New South Wales, Australia
Introduction: Polychemotherapy has been replaced by novel therapies in the management of Multiple Myeloma and is now reserved in the salvage setting despite limited published evidence. Commonly used regimens in this setting include D(T)-PACE and DCEP, which are multi-day continuous infusions, usually administered to patients with low comorbidities as inpatients. This study investigates the efficacy and safety of PCAB, a single day polychemotherapy in relapsed/refractory multiple myeloma (RRMM).
Methods: This multisite retrospective study involved four Australian tertiary hospitals. Patients with RRMM who received PCAB chemotherapy ± one novel agent between 1/1/2012-1/5/2023 were included. PCAB comprises of cyclophosphamide 600mg/m2, doxorubicin 30mg/m2 and carmustine 30mg/m2 day 1, and prednisone 60mg/m2 day 15, given every 28 days for up to 12 cycles. Baseline clinical characteristics, treatment response, adverse events and hospitalisation duration were recorded.
Results: Seventy-seven patients, median age 64 years (range 37-79) with median 4 (range 1-8) prior lines of therapy were included. Of these 76.6% had been exposed to both proteasome inhibitor and immunomodulatory drugs, and 63.6% had a previous autograft. Active extramedullary disease (EMD) and high-risk cytogenetics occurred in 35.1% and 58.0% of patients respectively. Forty-eight (62.3%) patients received only PCAB, while 29 (37.7%) received it in combination, most commonly with bortezomib (n=14) or thalidomide (n=7). After a median of 3 cycles (range 1-11), ORR was 38.4% (CR 5.5%) for the whole cohort, and 27.3% for those solely receiving PCAB. ORR in patients with EMD and high‐risk cytogenetics were 30.8% and 42.9% respectively. A subsequent therapy was received in 72.7% of patients, including as bridge to CAR-T therapy (n=2), autograft (n=3) and allograft (n=3). Median PFS and OS were 4.0 months and 6.7 months respectively.
Rate of any grade 3/4 cytopenia and febrile neutropenia was 76.2% and 44.3% respectively. Treatment-related deaths, all due to infections occurred in 6 patients (7.8%). Patients required inpatient management for a median of 3.6 days per 28 day cycle. Of patients who died, median 20.2% of days alive was spent as inpatient.
Conclusions: PCAB has retained efficacy in RRMM including those with high-risk cytogenetics and EMD. It may have a role as bridging therapy deliverable in an outpatient setting. Infection related mortalities highlight need for careful monitoring in this heavily pre-treated cohort.
Methods: This multisite retrospective study involved four Australian tertiary hospitals. Patients with RRMM who received PCAB chemotherapy ± one novel agent between 1/1/2012-1/5/2023 were included. PCAB comprises of cyclophosphamide 600mg/m2, doxorubicin 30mg/m2 and carmustine 30mg/m2 day 1, and prednisone 60mg/m2 day 15, given every 28 days for up to 12 cycles. Baseline clinical characteristics, treatment response, adverse events and hospitalisation duration were recorded.
Results: Seventy-seven patients, median age 64 years (range 37-79) with median 4 (range 1-8) prior lines of therapy were included. Of these 76.6% had been exposed to both proteasome inhibitor and immunomodulatory drugs, and 63.6% had a previous autograft. Active extramedullary disease (EMD) and high-risk cytogenetics occurred in 35.1% and 58.0% of patients respectively. Forty-eight (62.3%) patients received only PCAB, while 29 (37.7%) received it in combination, most commonly with bortezomib (n=14) or thalidomide (n=7). After a median of 3 cycles (range 1-11), ORR was 38.4% (CR 5.5%) for the whole cohort, and 27.3% for those solely receiving PCAB. ORR in patients with EMD and high‐risk cytogenetics were 30.8% and 42.9% respectively. A subsequent therapy was received in 72.7% of patients, including as bridge to CAR-T therapy (n=2), autograft (n=3) and allograft (n=3). Median PFS and OS were 4.0 months and 6.7 months respectively.
Rate of any grade 3/4 cytopenia and febrile neutropenia was 76.2% and 44.3% respectively. Treatment-related deaths, all due to infections occurred in 6 patients (7.8%). Patients required inpatient management for a median of 3.6 days per 28 day cycle. Of patients who died, median 20.2% of days alive was spent as inpatient.
Conclusions: PCAB has retained efficacy in RRMM including those with high-risk cytogenetics and EMD. It may have a role as bridging therapy deliverable in an outpatient setting. Infection related mortalities highlight need for careful monitoring in this heavily pre-treated cohort.
