Treatment of Newly Diagnosed Myeloma - Transplant Eligible
Poster Session 1
P-133: Validation of two International Myeloma Staging Systems: Second Revision of ISS and Mayo Additive Staging Sytems (MASS) in an external cohort of Ankara University
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Guldane Cengiz Seval, MD
Assoc. Prof.
Ankara University School of Medicine, Department of Hematology, Ankara, Turkey
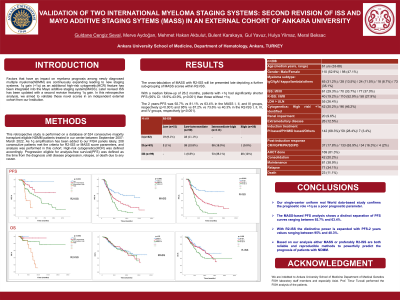
Introduction: Factors that have an impact on myeloma prognosis among newly diagnosed multiple myeloma(NDMM) are continuously expanding leading to new staging systems. 1q gain (+1q) as an additional high-risk cytogenetic(HCR) feature has been integrated into the Mayo additive staging system(MASS). Later revised ISS has been updated with a second revision featuring 1q gain. In this retrospective analysis, we aimed to validate these novel scores in an independent external cohort from our Institution.
Methods: This retrospective study is performed on a database of 524 consecutive majority transplant eligible NDMM patients treated in our center between September 2007- March 2022. As 1q amplification has been added to our FISH panels lately, 208 consecutive patients met the criteria for R2-ISS or MASS score parameters, and analysis was performed in this cohort. High-risk cytogenetics(HCR) was defined accordingly. Progression eligible for analysis-free survival(PFS) was defined as the time from the diagnosis until disease progression, relapse, or death due to any cause.
Results: Patients (median age 61 years (33-88 years); (female/male: 47.1%/52.9% ) received either bortezomib-based triplet (96.7%) without (n:142) or with an immunomodulatory drug (28.4%) as induction therapy. Out of the 208 patients, 169 patients underwent autologous hematopoietic stem cell transplantation (AHCT). As a post-ASCT treatment, consolidation (20.2%) and maintenance (38.9%) were given to patients. The median follow-up for all patients is 19.8 months (range: 3-237 mos). HCR was detected in 42 patients (20.2%) with an additional +1q identified among 96 cases, accounting for 46.2% of 208 patients. Based on the calculation of risk score in MASS; 42 patients (20.2%) ranked as score 0 (MASS I), 67 patients (32.2%) score 1 (MASS II) and 99 patients (47.6%) score +2 (MASS III). The cross-tabulation of MASS with R2-ISS will be presented late depicting a further sub-grouping of MASS scores within R2-ISS. With a median follow-up of 26.2 months, patients with +1q had significantly shorter PFS (95% CI: 18.9%-43.9%, p< 0.001) than those without +1q. The 2 years-PFS was 92.7% vs 81.1% vs 63.4% in the MASS I, II, and III groups, respectively (p < 0.001) and 95% vs 87.2% vs 73.6% vs 40.3% in the R2-ISS I, II, III, and IV groups, respectively (p < 0.001).
Conclusions: Our single-center uniform real World data-based study confirms the prognostic role +1q as a poor prognostic parameter. The MASS-based PFS analysis shows a distinct separation of PFS curves ranging between 92.7% and 63.4%. With R2-ISS the distinctive power is expanded with PFS-2 years values ranging between 95% and 40.3%. Based on our analysis either MASS or preferably R2-ISS are both reliable and reproducible methods to powerfully predict the prognosis of patients with NDMM.
Methods: This retrospective study is performed on a database of 524 consecutive majority transplant eligible NDMM patients treated in our center between September 2007- March 2022. As 1q amplification has been added to our FISH panels lately, 208 consecutive patients met the criteria for R2-ISS or MASS score parameters, and analysis was performed in this cohort. High-risk cytogenetics(HCR) was defined accordingly. Progression eligible for analysis-free survival(PFS) was defined as the time from the diagnosis until disease progression, relapse, or death due to any cause.
Results: Patients (median age 61 years (33-88 years); (female/male: 47.1%/52.9% ) received either bortezomib-based triplet (96.7%) without (n:142) or with an immunomodulatory drug (28.4%) as induction therapy. Out of the 208 patients, 169 patients underwent autologous hematopoietic stem cell transplantation (AHCT). As a post-ASCT treatment, consolidation (20.2%) and maintenance (38.9%) were given to patients. The median follow-up for all patients is 19.8 months (range: 3-237 mos). HCR was detected in 42 patients (20.2%) with an additional +1q identified among 96 cases, accounting for 46.2% of 208 patients. Based on the calculation of risk score in MASS; 42 patients (20.2%) ranked as score 0 (MASS I), 67 patients (32.2%) score 1 (MASS II) and 99 patients (47.6%) score +2 (MASS III). The cross-tabulation of MASS with R2-ISS will be presented late depicting a further sub-grouping of MASS scores within R2-ISS. With a median follow-up of 26.2 months, patients with +1q had significantly shorter PFS (95% CI: 18.9%-43.9%, p< 0.001) than those without +1q. The 2 years-PFS was 92.7% vs 81.1% vs 63.4% in the MASS I, II, and III groups, respectively (p < 0.001) and 95% vs 87.2% vs 73.6% vs 40.3% in the R2-ISS I, II, III, and IV groups, respectively (p < 0.001).
Conclusions: Our single-center uniform real World data-based study confirms the prognostic role +1q as a poor prognostic parameter. The MASS-based PFS analysis shows a distinct separation of PFS curves ranging between 92.7% and 63.4%. With R2-ISS the distinctive power is expanded with PFS-2 years values ranging between 95% and 40.3%. Based on our analysis either MASS or preferably R2-ISS are both reliable and reproducible methods to powerfully predict the prognosis of patients with NDMM.
