Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-277: Venetoclax Versus Bortezomib, in Combination with Daratumumab and Dexamethasone, in Patients With t(11;14)-Positive Relapsed or Refractory Multiple Myeloma
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Jonathan L. Kaufman, MD
Professor of Hematology and Medical Oncology
Winship Cancer Institute of Emory University
Atlanta, Georgia, United States
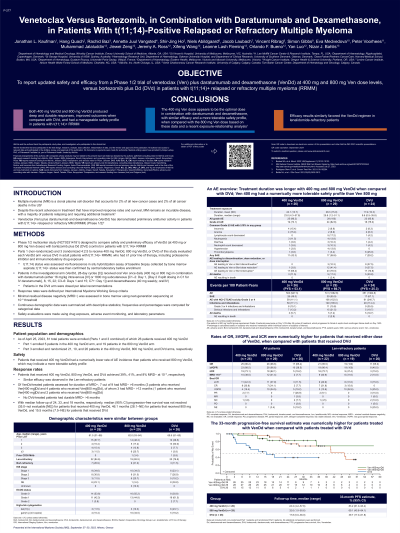
Introduction: Venetoclax (Ven) plus daratumumab and dexamethasone (VenDd) has demonstrated preliminary antitumor activity in patients (pts) with t(11;14)+ relapsed/refractory multiple myeloma (RRMM; Phase 1/2). Here, we report updated safety and efficacy from this Phase1/2 trial of VenDd at 400 and 800 mg Ven dose levels, versus bortezomib plus Dd (DVd) in pts with t(11;14)+ RRMM.
Methods: Parts 1 (nonrandomized) and 3 (randomized among 400 mg VenDd, 800 mg VenDd and DVd arms) in this Phase 1/2 multicenter study evaluated VenDd versus DVd in pts with t(11;14)+ RRMM, who had ≥1 prior line of therapy (LOT), including proteasome inhibitor and immunomodulatory drug exposure (NCT03314181). Pts in the investigational arm (VenDd, 28 day [D] cycles [C]) received oral Ven once daily (400 mg or 800 mg) with daratumumab (either 16 mg/kg IV or 1800 mg subcutaneous [C1–2: D1, {D2 if split dosing in C1 for IV daratumumab}, 8, 15, 22; C3–6: D1 and 15; C7+: D1]) and dexamethasone (40 mg weekly; oral/IV); pts in the DVd arm were dosed per label recommendations. Overall response rate (ORR) was defined as ≥partial response per IMWG criteria. Minimal residual disease negativity (MRD˗) was assessed in bone marrow using next-generation sequencing. This trial was designed to compare safety and preliminary efficacy of VenDd (at 400 or 800 mg Ven doses) with DVd (control).
Results: Part 1 enrolled 5 pts (400 mg VenDd) and 19 pts (800 mg VenDd). Part 3 enrolled 21, 10, and 26 pts in the 400 mg VenDd, 800 mg VenDd and DVd arms. As of Mar 10, 2023, 80 total pts were enrolled (Parts 1 and 3 combined); 55 pts received VenDd (11% del17p, 13% 1q21abn; 53% 1 prior LOT, 2% prior anti-CD38 mAb); and 24 received DVd (21% del17p; 38% 1 prior LOT, 4% anti-CD38 mAb). Median (range) follow-up and treatment exposure (months) were longer with VenDd than Dvd (28.2 [1.0–55.7] and 23.3 [1.2–56.3] with VenDd vs 16.9 [0.0–34.1] and 9.6 [0.5–33.9] with DVd). The most common AEs (>30%) with DVd were diarrhea, insomnia, and fatigue, and with VenDd were those plus nausea, upper respiratory tract infection, and COVID-19. SAE rates were 51% (VenDd) and 25% (DVd). Discontinuation due to AEs occurred with 6% of pts with VenDd (none with DVd). VenDd achieved 96% ORR, 93% ≥VGPR, 67% ≥CR, 35% MRD˗ at 10^-5 and median PFS not reached (95% CI: 35.0–NE). DVd achieved: 65% ORR, 39% ≥VGPR, 19% ≥CR, 8% MRD˗ at 10^-5, and median PFS 15.5 months (7.5–NE). The 33-month PFS rate was 73.4% (95% CI: 56.4–84.6) vs 38.8% (16.3–61.1) for VenDd vs DVd. Of 8 VenDd-treated pts assessed for duration of MRD˗, 6 had MRD˗ >6 months, of whom 2 had MRD˗ >12 months. No DVd-treated pts had durable MRD˗ >6 months.
Conclusions: VenDd produced deep and durable responses, improved outcomes compared with DVd, and had a manageable safety profile in pts with t(11;14)+ RRMM. Data supporting Venetoclax dose selection will be presented.
Methods: Parts 1 (nonrandomized) and 3 (randomized among 400 mg VenDd, 800 mg VenDd and DVd arms) in this Phase 1/2 multicenter study evaluated VenDd versus DVd in pts with t(11;14)+ RRMM, who had ≥1 prior line of therapy (LOT), including proteasome inhibitor and immunomodulatory drug exposure (NCT03314181). Pts in the investigational arm (VenDd, 28 day [D] cycles [C]) received oral Ven once daily (400 mg or 800 mg) with daratumumab (either 16 mg/kg IV or 1800 mg subcutaneous [C1–2: D1, {D2 if split dosing in C1 for IV daratumumab}, 8, 15, 22; C3–6: D1 and 15; C7+: D1]) and dexamethasone (40 mg weekly; oral/IV); pts in the DVd arm were dosed per label recommendations. Overall response rate (ORR) was defined as ≥partial response per IMWG criteria. Minimal residual disease negativity (MRD˗) was assessed in bone marrow using next-generation sequencing. This trial was designed to compare safety and preliminary efficacy of VenDd (at 400 or 800 mg Ven doses) with DVd (control).
Results: Part 1 enrolled 5 pts (400 mg VenDd) and 19 pts (800 mg VenDd). Part 3 enrolled 21, 10, and 26 pts in the 400 mg VenDd, 800 mg VenDd and DVd arms. As of Mar 10, 2023, 80 total pts were enrolled (Parts 1 and 3 combined); 55 pts received VenDd (11% del17p, 13% 1q21abn; 53% 1 prior LOT, 2% prior anti-CD38 mAb); and 24 received DVd (21% del17p; 38% 1 prior LOT, 4% anti-CD38 mAb). Median (range) follow-up and treatment exposure (months) were longer with VenDd than Dvd (28.2 [1.0–55.7] and 23.3 [1.2–56.3] with VenDd vs 16.9 [0.0–34.1] and 9.6 [0.5–33.9] with DVd). The most common AEs (>30%) with DVd were diarrhea, insomnia, and fatigue, and with VenDd were those plus nausea, upper respiratory tract infection, and COVID-19. SAE rates were 51% (VenDd) and 25% (DVd). Discontinuation due to AEs occurred with 6% of pts with VenDd (none with DVd). VenDd achieved 96% ORR, 93% ≥VGPR, 67% ≥CR, 35% MRD˗ at 10^-5 and median PFS not reached (95% CI: 35.0–NE). DVd achieved: 65% ORR, 39% ≥VGPR, 19% ≥CR, 8% MRD˗ at 10^-5, and median PFS 15.5 months (7.5–NE). The 33-month PFS rate was 73.4% (95% CI: 56.4–84.6) vs 38.8% (16.3–61.1) for VenDd vs DVd. Of 8 VenDd-treated pts assessed for duration of MRD˗, 6 had MRD˗ >6 months, of whom 2 had MRD˗ >12 months. No DVd-treated pts had durable MRD˗ >6 months.
Conclusions: VenDd produced deep and durable responses, improved outcomes compared with DVd, and had a manageable safety profile in pts with t(11;14)+ RRMM. Data supporting Venetoclax dose selection will be presented.
