Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-226: Safety and clinical activity of belantamab mafodotin combined with carfilzomib, lenalidomide, and dexamethasone after at least one prior line of therapy, interim results from phase 1 clinical trial.
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Shebli Atrash, MD
hematology & oncology
Levine Cancer Institute
Charlotte, North Carolina, United States
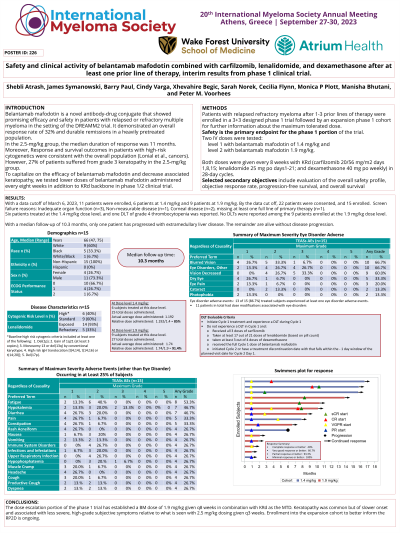
Introduction: Belantamab mafodotin (BM) is a novel BCMA-targeted antibody-drug conjugate that showed promising efficacy in relapsed/refractory multiple myeloma (RRMM) patients (pts), with an overall response rate (ORR) of 32% and median duration of response (DOR) of 11 months when dosed at 2.5 mg/kg q3 weeks—however, 27% of pts suffered from G3 keratopathy. Preliminary clinical data support the use of BM with a proteasome inhibitor and IMiD-based therapy. To capitalize on the efficacy of BM and decrease keratopathy, we conducted a phase 1/2 clinical trial evaluating lower doses of BM administered q8 weeks in combination with the KRd backbone for pts with early relapse of MM.
Methods: Pts with RRMM after 1-3 prior lines of therapy (LOT) were enrolled in a phase 1 trial with a 3+3 dose escalation followed by an expansion cohort to better inform the recommended phase II dose (RP2D). The primary objective for the phase 1 portion of the trial was to establish the maximum tolerated dose (MTD) of BM when given with KRd as determined by dose-limiting toxicities (DLTs) in cycle 1. Secondary objectives included ORR, depth of response, DOR, progression-free survival, overall survival, and safety. Two doses of BM were tested: 1.4 mg/kg and 1.9 mg/kg given IV over 30 – 60 minutes every 8 weeks with KRd (K 20/56 mg/m2 days 1,8,15; R 25 mg po days1-21; and d 20/40 mg po weekly) in 28-day cycles for up to 18 cycles followed by R maintenance.
Results: With a data cutoff of March 6, 2023, 11 pts were enrolled, 6 pts at 1.4 mg/kg and 5 pts at 1.9 mg/kg. 63.6% of pts were male, 45.5% black, and 18% had high-risk cytogenetics and 64% including 1q gain. 91% were refractory to a maintenance dose of R, all were bortezomib exposed, and 27% were daratumumab refractory. The median LOT was 1 (range 1-3 ).
All 11 enrolled pts were DLT evaluable. At the 1.4 mg/kg dose level, one DLT of grade 4 thrombocytopenia was reported out of 6 pts. No DLTs were reported among the pts enrolled at the 1.9 mg/kg dose level (including a 6th pt treated after data cutoff). The most common adverse events were non-specified eye disorders (81.1%), blurred vision (63.6%), hypokalemia (63.6%), diarrhea (63.6%), fatigue (63.6%), constipation (45.5%), and pain (45.5%). Four pts experienced G3 keratopathy, and the median time to recovery was 25 days (range 8-29 days ). All pts achieved at least a PR, the VGPR(+) rate was 73%, and the CR(+) rate was 45%. With a median follow-up of 9.2 months, only one pt has progressed with extramedullary liver disease. The remainders are alive without disease progression.
Conclusions: The dose escalation portion of the phase 1 trial has established a BM dose of 1.9 mg/kg given q8 weeks in combination with KRd as the MTD. Keratopathy was common but of slower onset and associated with less severe, high-grade subjective symptoms relative to what is seen with 2.5 mg/kg dosing given q3 weeks. Enrollment into the expansion cohort to better inform the RP2D is ongoing, and updated data will be presented at the meeting.
Methods: Pts with RRMM after 1-3 prior lines of therapy (LOT) were enrolled in a phase 1 trial with a 3+3 dose escalation followed by an expansion cohort to better inform the recommended phase II dose (RP2D). The primary objective for the phase 1 portion of the trial was to establish the maximum tolerated dose (MTD) of BM when given with KRd as determined by dose-limiting toxicities (DLTs) in cycle 1. Secondary objectives included ORR, depth of response, DOR, progression-free survival, overall survival, and safety. Two doses of BM were tested: 1.4 mg/kg and 1.9 mg/kg given IV over 30 – 60 minutes every 8 weeks with KRd (K 20/56 mg/m2 days 1,8,15; R 25 mg po days1-21; and d 20/40 mg po weekly) in 28-day cycles for up to 18 cycles followed by R maintenance.
Results: With a data cutoff of March 6, 2023, 11 pts were enrolled, 6 pts at 1.4 mg/kg and 5 pts at 1.9 mg/kg. 63.6% of pts were male, 45.5% black, and 18% had high-risk cytogenetics and 64% including 1q gain. 91% were refractory to a maintenance dose of R, all were bortezomib exposed, and 27% were daratumumab refractory. The median LOT was 1 (range 1-3 ).
All 11 enrolled pts were DLT evaluable. At the 1.4 mg/kg dose level, one DLT of grade 4 thrombocytopenia was reported out of 6 pts. No DLTs were reported among the pts enrolled at the 1.9 mg/kg dose level (including a 6th pt treated after data cutoff). The most common adverse events were non-specified eye disorders (81.1%), blurred vision (63.6%), hypokalemia (63.6%), diarrhea (63.6%), fatigue (63.6%), constipation (45.5%), and pain (45.5%). Four pts experienced G3 keratopathy, and the median time to recovery was 25 days (range 8-29 days ). All pts achieved at least a PR, the VGPR(+) rate was 73%, and the CR(+) rate was 45%. With a median follow-up of 9.2 months, only one pt has progressed with extramedullary liver disease. The remainders are alive without disease progression.
Conclusions: The dose escalation portion of the phase 1 trial has established a BM dose of 1.9 mg/kg given q8 weeks in combination with KRd as the MTD. Keratopathy was common but of slower onset and associated with less severe, high-grade subjective symptoms relative to what is seen with 2.5 mg/kg dosing given q3 weeks. Enrollment into the expansion cohort to better inform the RP2D is ongoing, and updated data will be presented at the meeting.
