Myeloma Genomics and cell signaling
Poster Session 3
P-366: Signaling Pathway Data Analytics of Nephropathy and Neuropathy from Drug Toxicities in Multiple Myeloma
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Shahzad Raza, MD (he/him/his)
Staff
Taussig Cancer Institute, Cleveland Clinic, United States
Introduction: With the emergence of new therapeutic options, it is crucial to gain a comprehensive understanding of the toxicity profile associated with anti-multiple myeloma (MM) drug regimens (AMDRs). Previous studies have indicated that the occurrence of adverse events (AEs) may be influenced by specific genes and genetic factors. This study aims to investigate the link between genes, drug regimens, and AEs in AMDRs. By exploring the genetic evidence of neuro and renal AEs associated with specific regimens, we aim to understand the interplay between genetics and treatment-related toxicity in MM patients.
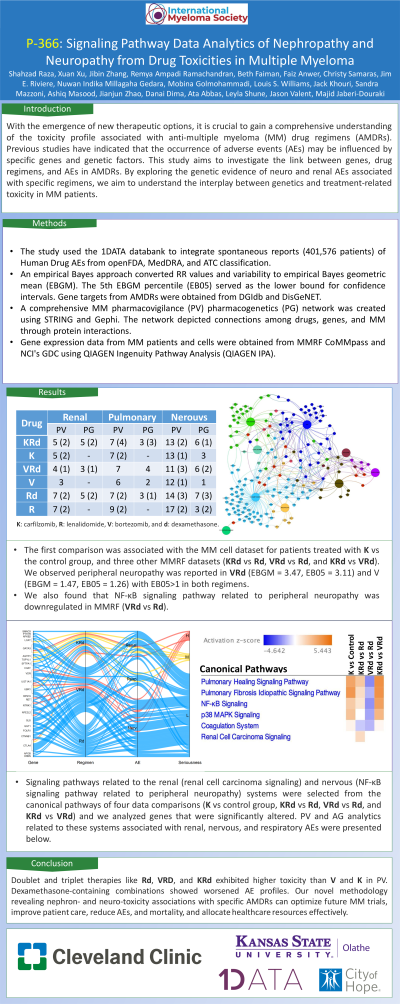
Methods: The study used the 1DATA databank to integrate spontaneous reports (401,576 patients) of Human Drug AEs from openFDA, MedDRA, and ATC classification. An empirical Bayes approach converted RR values and variability to empirical Bayes geometric mean (EBGM). The 5th EBGM percentile (EB05) served as the lower bound for confidence intervals. Gene targets from AMDRs were obtained from DGIdb and DisGeNET. A comprehensive MM pharmacovigilance (PV) pharmacogenetics (PG) network was created using STRING and Gephi. The network depicted connections among drugs, genes, and MM through protein interactions. Gene expression data from MM patients and cells were obtained from MMRF CoMMpass and NCI's GDC using QIAGEN Ingenuity Pathway Analysis (QIAGEN IPA).
Results: The first comparison was associated with the MM cell dataset for patients treated with K vs the control group, and three other MMRF datasets (KRd vs Rd, VRd vs Rd, and KRd vs VRd). We observed peripheral neuropathy was reported in VRd (EBGM = 3.47, EB05 = 3.11) and V (EBGM = 1.47, EB05 = 1.26) with EB05>1 in both regimens. We also found that NF-κB signaling pathway related to peripheral neuropathy was downregulated in MMRF (VRd vs Rd). Next, signaling pathways related to the renal (renal cell carcinoma signaling) and nervous (NF-κB signaling pathway related to peripheral neuropathy) systems were selected from the canonical pathways of four data comparisons (K vs control group, KRd vs Rd, VRd vs Rd, and KRd vs VRd) and we analyzed genes that were significantly altered. PV and PG analytics related to these systems associated with renal, nervous, and respiratory AEs were presented below.
Drug EBGM>1 (EB05>1)
Renal Respiratory Nervous
PV PG PV PG PV PG
KRd 5 (2) 5 (2) 7 (4) 3 (3) 13 (2) 6 (1)
K 5 (2) - 7 (2) - 13 (1) 3
VRd 4 (1) 3 (1) 7 4 11 (3) 6 (2)
V 3 - 6 2 12 (1) 1
Rd 7 (2) 5 (2) 7 (2) 3 (1) 14 (3) 7 (3)
R 7 (2) - 9 (2) - 17 (2) 3 (2)
K: carfilzomib, R: lenalidomide, V: bortezomib, and d: dexamethasone.
Conclusions: Doublet and triplet therapies like Rd, VRD, and KRd exhibited higher toxicity than V and K in PV. Dexamethasone-containing combinations showed worsened AE profiles. This novel methodology revealing nephro- and neuro-toxicity associations with specific AMDRs can potentially mitigate AEs and improve treatment tolerability.
Methods: The study used the 1DATA databank to integrate spontaneous reports (401,576 patients) of Human Drug AEs from openFDA, MedDRA, and ATC classification. An empirical Bayes approach converted RR values and variability to empirical Bayes geometric mean (EBGM). The 5th EBGM percentile (EB05) served as the lower bound for confidence intervals. Gene targets from AMDRs were obtained from DGIdb and DisGeNET. A comprehensive MM pharmacovigilance (PV) pharmacogenetics (PG) network was created using STRING and Gephi. The network depicted connections among drugs, genes, and MM through protein interactions. Gene expression data from MM patients and cells were obtained from MMRF CoMMpass and NCI's GDC using QIAGEN Ingenuity Pathway Analysis (QIAGEN IPA).
Results: The first comparison was associated with the MM cell dataset for patients treated with K vs the control group, and three other MMRF datasets (KRd vs Rd, VRd vs Rd, and KRd vs VRd). We observed peripheral neuropathy was reported in VRd (EBGM = 3.47, EB05 = 3.11) and V (EBGM = 1.47, EB05 = 1.26) with EB05>1 in both regimens. We also found that NF-κB signaling pathway related to peripheral neuropathy was downregulated in MMRF (VRd vs Rd). Next, signaling pathways related to the renal (renal cell carcinoma signaling) and nervous (NF-κB signaling pathway related to peripheral neuropathy) systems were selected from the canonical pathways of four data comparisons (K vs control group, KRd vs Rd, VRd vs Rd, and KRd vs VRd) and we analyzed genes that were significantly altered. PV and PG analytics related to these systems associated with renal, nervous, and respiratory AEs were presented below.
Drug EBGM>1 (EB05>1)
Renal Respiratory Nervous
PV PG PV PG PV PG
KRd 5 (2) 5 (2) 7 (4) 3 (3) 13 (2) 6 (1)
K 5 (2) - 7 (2) - 13 (1) 3
VRd 4 (1) 3 (1) 7 4 11 (3) 6 (2)
V 3 - 6 2 12 (1) 1
Rd 7 (2) 5 (2) 7 (2) 3 (1) 14 (3) 7 (3)
R 7 (2) - 9 (2) - 17 (2) 3 (2)
K: carfilzomib, R: lenalidomide, V: bortezomib, and d: dexamethasone.
Conclusions: Doublet and triplet therapies like Rd, VRD, and KRd exhibited higher toxicity than V and K in PV. Dexamethasone-containing combinations showed worsened AE profiles. This novel methodology revealing nephro- and neuro-toxicity associations with specific AMDRs can potentially mitigate AEs and improve treatment tolerability.
