Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-286: Impact of hypogammaglobulinemia and immunoglobulin replacement therapy on infection rate in patients with RRMM treated with elranatamab: Post-hoc analysis from MagnetisMM-3
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Xavier P. Leleu, MD, PhD (he/him/his)
Head of Myeloma Clinic and Head of Department of Haematology
Hospital La Mileterie, Poitiers, France
Poitiers, United States
Introduction: Patients (pts) with RRMM are at increased risk for severe infections due to immunosuppression related to underlying MM as well as anti-MM therapies. As a result, management guidelines include recommendations for anti-infective prophylaxis in high-risk pts, including immunoglobulin (Ig) replacement therapy for hypogammaglobulinemia. However, sparse data exist demonstrating the impact of Ig replacement on the incidence of infection in this population.
Methods: A post-hoc analysis evaluating the impact of Ig replacement and hypogammaglobulinema on infections was conducted in pts enrolled in MagnetisMM-3 (NCT04649359), a Phase 2 study of SC elranatamab (BCMA x CD3 bispecific mAb) in pts with RRMM. Exposure adjusted infection rates (EAIR) in the following subgroups were analyzed: On vs Off Ig replacement therapy (n=187); Without vs With hypogammaglobulinemia (in pts with quantitative Ig data available, n=137). Infection events were defined as any distinct infection event or as any in increase in grade in a single infection event. “On Ig” period was defined as the period between the administration of Ig replacement + 30 days. Hypogammaglobulinemia was defined as IgG < 400 mg/dL. For pts with non-IgG myeloma, quantitative IgG results were used. For pts with IgG myeloma, functional IgG levels were determined by subtracting the M-spike in SPEP from the quantitative IgG result. EAIR were calculated as the number infection events in each period divided by the total time in months in each period.
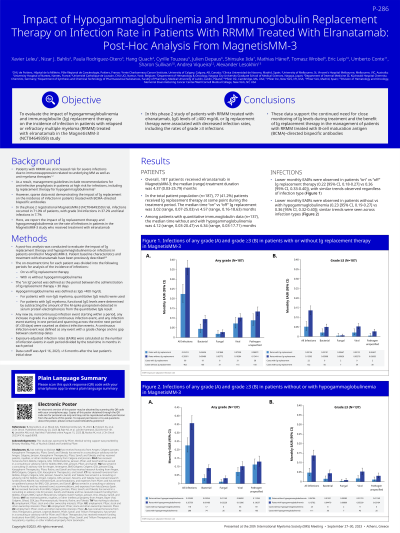
Results: 187 pts received elranatamab. At baseline, among pts with baseline quantitative Ig data available (n=124), 93.5% had immune paresis (defined as ≥2 uninvolved Ig < LLN); 41.2% of pts received Ig replacement during the treatment period. The median (range) time On and Off Ig replacement was 4.0 (0.3, 26.2) and 5.0 (0.6, 20.5) months respectively, while the median (range) time without and with hypogammaglobulinemia was 4.9 (0.03, 23.1) and 6.9 (0.9, 19.1). The monthly EAIR in pts On vs Off Ig replacement were 0.162 (95% CI: 0.128, 0.203) vs 0.305 (95% CI: 0.275, 0.337) for any grade infection, and 0.041 (95% CI: 0.025, 0.064) vs 0.116 (95% CI: 0.098, 0.136) for Grade ≥3 infection, respectively. In pts without vs with hypogammaglobulinemia, the monthly EAIR were 0.182 (95% CI: 0.150, 0.219) vs 0.307 (95% CI: 0.271, 0.354) for any grade infection, and 0.039 (95% CI: 0.025, 0.059) vs 0.122 (95% CI: 0.100, 0.147) for Grade ≥3 infection, respectively. Similar results were observed across infection types (bacterial, fungal, viral).
Conclusions: In this Phase 2 study of pts with RRMM treated with elranatamab, IgG levels ≥400 mg/dL or Ig replacement therapy were associated with a decreased infection rate, including the rate of Grade ≥3 infections. These data support the continued need for close monitoring of Ig levels during treatment and the benefit of Ig replacement therapy in the management of pts with RRMM treated with BCMA-directed bispecific antibodies.
Methods: A post-hoc analysis evaluating the impact of Ig replacement and hypogammaglobulinema on infections was conducted in pts enrolled in MagnetisMM-3 (NCT04649359), a Phase 2 study of SC elranatamab (BCMA x CD3 bispecific mAb) in pts with RRMM. Exposure adjusted infection rates (EAIR) in the following subgroups were analyzed: On vs Off Ig replacement therapy (n=187); Without vs With hypogammaglobulinemia (in pts with quantitative Ig data available, n=137). Infection events were defined as any distinct infection event or as any in increase in grade in a single infection event. “On Ig” period was defined as the period between the administration of Ig replacement + 30 days. Hypogammaglobulinemia was defined as IgG < 400 mg/dL. For pts with non-IgG myeloma, quantitative IgG results were used. For pts with IgG myeloma, functional IgG levels were determined by subtracting the M-spike in SPEP from the quantitative IgG result. EAIR were calculated as the number infection events in each period divided by the total time in months in each period.
Results: 187 pts received elranatamab. At baseline, among pts with baseline quantitative Ig data available (n=124), 93.5% had immune paresis (defined as ≥2 uninvolved Ig < LLN); 41.2% of pts received Ig replacement during the treatment period. The median (range) time On and Off Ig replacement was 4.0 (0.3, 26.2) and 5.0 (0.6, 20.5) months respectively, while the median (range) time without and with hypogammaglobulinemia was 4.9 (0.03, 23.1) and 6.9 (0.9, 19.1). The monthly EAIR in pts On vs Off Ig replacement were 0.162 (95% CI: 0.128, 0.203) vs 0.305 (95% CI: 0.275, 0.337) for any grade infection, and 0.041 (95% CI: 0.025, 0.064) vs 0.116 (95% CI: 0.098, 0.136) for Grade ≥3 infection, respectively. In pts without vs with hypogammaglobulinemia, the monthly EAIR were 0.182 (95% CI: 0.150, 0.219) vs 0.307 (95% CI: 0.271, 0.354) for any grade infection, and 0.039 (95% CI: 0.025, 0.059) vs 0.122 (95% CI: 0.100, 0.147) for Grade ≥3 infection, respectively. Similar results were observed across infection types (bacterial, fungal, viral).
Conclusions: In this Phase 2 study of pts with RRMM treated with elranatamab, IgG levels ≥400 mg/dL or Ig replacement therapy were associated with a decreased infection rate, including the rate of Grade ≥3 infections. These data support the continued need for close monitoring of Ig levels during treatment and the benefit of Ig replacement therapy in the management of pts with RRMM treated with BCMA-directed bispecific antibodies.
