Treatment of Newly Diagnosed Myeloma - Transplant Eligible
Poster Session 1
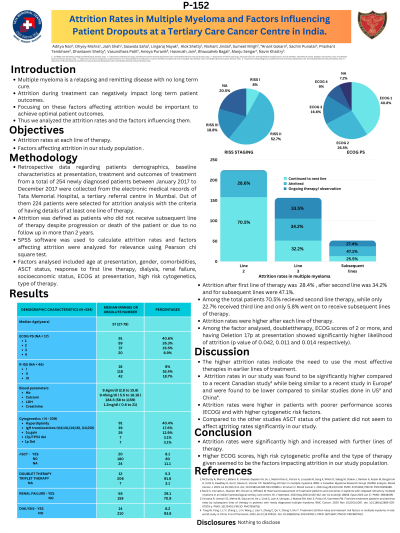
P-152: Attrition Rates in Multiple Myeloma and factors influencing patient dropouts at a tertiary referral center in India.
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST
ADITYA RANJITHKUMAR NAIR (he/him/his)
3rd MBBS STUDENT
SETH GS MEDICAL COLLEGE AND KEM HOSPITAL,MUMBAI
Mumbai, Maharashtra, India
Introduction: Because of its relapsing-remitting nature and no long-term cure, patients with multiple myeloma require extended therapy with chemotherapy, novel agents, monoclonal antibodies, and autologous stem cell transplants (ASCT) for optimal outcomes. Attrition during treatment can negatively impact long-term outcomes and factors influencing the same may be important to focus on to achieve optimal patient outcomes. This study aims to examine attrition rates and the factors influencing them.
Methods: This retrospective study analyzed data from 224 newly diagnosed patients of multiple myeloma from January 2017 to December 2017 at TMH, Mumbai. The patients included had received or were started on at least one line of therapy. The patient factors such as age, co-morbidities, clinical and laboratory evaluations were recorded along with the lines of therapy (LOTs) received, best response, and therapies received including ASCT. Factors predicting attrition were analyzed using a chi-squared test in two groups using SPSS version 22.
Results: Among the newly diagnosed patients during the study period, the median age was 57 years, with 67.1 % being male. The most common 1st line therapy given was Bortezomib, cyclophosphamide, and dexamethasone combination (76.4% of patients). The attrition rates among the patients were 28.6% for the second LOT, 33.8 % for the 3rd LOT, and 45.3% for the subsequent LOTs. Among the people who dropped out for the second LOT, only 3% of patients had received ASCT, 18.8% of patients had received maintenance post 1st LOT, 2% had associated co-morbidities, 37.5% had renal dysfunction, 46.9% patients were ISS stage III at diagnosis and 28.1% patients had high-risk cytogenetics at presentation. In the group who received second LOT or higher, 11.2% of the patients received ASCT, 27.3 % had received maintenance post 1st LOT, 68.3% had received Radiotherapy, 34.2 % had associated co-morbidities, renal dysfunction was present in 25.5% of the patients, 46% of the patients were ISS stage III at diagnosis and 25.5% patients had high-risk cytogenetics at presentation. Among the factor analyzed, doublet therapy, ECOG scores of 2 or more, and having Del17p at presentation showed a significantly higher likelihood of attrition (p-value of 0.042, 0.011, and 0.014 respectively). The median Overall Survival (OS) was 3.9 years (95% Confidence Interval 3.3 years – 4.6 years). The median Overall Survival (OS) for people who dropped out after first-line of therapy was 1 year (95% Confidence Interval 0.6 years – 1.5 years) compared to an OS of 5.6 years (95% Confidence Interval 5.1 years – 6.0 years) in patients who did receive second-line therapy.
Conclusions: Our study shows a significant proportion of patients did not receive subsequent lines of therapy in our clinical setting and have inferior survival. Most effective therapies should be used in earlier lines to benefit patients from all available treatment modalities.
Methods: This retrospective study analyzed data from 224 newly diagnosed patients of multiple myeloma from January 2017 to December 2017 at TMH, Mumbai. The patients included had received or were started on at least one line of therapy. The patient factors such as age, co-morbidities, clinical and laboratory evaluations were recorded along with the lines of therapy (LOTs) received, best response, and therapies received including ASCT. Factors predicting attrition were analyzed using a chi-squared test in two groups using SPSS version 22.
Results: Among the newly diagnosed patients during the study period, the median age was 57 years, with 67.1 % being male. The most common 1st line therapy given was Bortezomib, cyclophosphamide, and dexamethasone combination (76.4% of patients). The attrition rates among the patients were 28.6% for the second LOT, 33.8 % for the 3rd LOT, and 45.3% for the subsequent LOTs. Among the people who dropped out for the second LOT, only 3% of patients had received ASCT, 18.8% of patients had received maintenance post 1st LOT, 2% had associated co-morbidities, 37.5% had renal dysfunction, 46.9% patients were ISS stage III at diagnosis and 28.1% patients had high-risk cytogenetics at presentation. In the group who received second LOT or higher, 11.2% of the patients received ASCT, 27.3 % had received maintenance post 1st LOT, 68.3% had received Radiotherapy, 34.2 % had associated co-morbidities, renal dysfunction was present in 25.5% of the patients, 46% of the patients were ISS stage III at diagnosis and 25.5% patients had high-risk cytogenetics at presentation. Among the factor analyzed, doublet therapy, ECOG scores of 2 or more, and having Del17p at presentation showed a significantly higher likelihood of attrition (p-value of 0.042, 0.011, and 0.014 respectively). The median Overall Survival (OS) was 3.9 years (95% Confidence Interval 3.3 years – 4.6 years). The median Overall Survival (OS) for people who dropped out after first-line of therapy was 1 year (95% Confidence Interval 0.6 years – 1.5 years) compared to an OS of 5.6 years (95% Confidence Interval 5.1 years – 6.0 years) in patients who did receive second-line therapy.
Conclusions: Our study shows a significant proportion of patients did not receive subsequent lines of therapy in our clinical setting and have inferior survival. Most effective therapies should be used in earlier lines to benefit patients from all available treatment modalities.
