Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-313: ALLG MM25 (VIBER-M): A Phase Ib/II study of Venetoclax, Iberdomide and Dexamethasone for patients in first or second relapse of Multiple Myeloma with t(11;14)
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Shirlene S. Sim, MBBS(Hons) BMedSc FRACP FRCPA (she/her/hers)
Consultant Haematologist
St Vincent's Hospital Melbourne, VIC, Australia
Fitzroy, Victoria, Australia
Introduction: Translocation t(11;14) is an initiating lesion that is seen in approximately 20% of patients with multiple myeloma (MM). It is considered an intermediate-risk lesion and is associated with inferior outcomes amongst the intermediate risk-group. This is the only cytogenetic lesion in MM that is amenable to targeted treatment with Bcl2-inhibition. Venetoclax (Ven) is a Bcl2-inhibitor that induces cell death, and has been shown to be highly efficacious in patients with relapsed/refractory myeloma (RRMM) who harbour t(11;14) and high Bcl2 levels. Given that there is a significant attrition rate in patient numbers with each subsequent line of therapy, there is a need to move Bcl2-inhibitors to earlier lines of treatment to optimise clinical outcomes.
In the current era where lenalidomide (len) maintenance is used in first line, there is a need for a len-free regimen at relapse. Iberdomide is a potent cereblon E3 ligase modulator (CELMod) that has been shown in pre-clinical studies to have direct anti-myeloma and immunostimulatory activity, including in len- and pomalidomide-resistant cell lines. Early studies in heavily pre-treated RRMM have demonstrated good response rates when iberdomide is combined with standard-of-care therapy.
We hypothesize that the combination of Ven, iberdomide (Iber) and dexamethasone (Dex) will be highly synergistic and have better utility in rescuing MM patients with t(11;14) at first or second relapse.
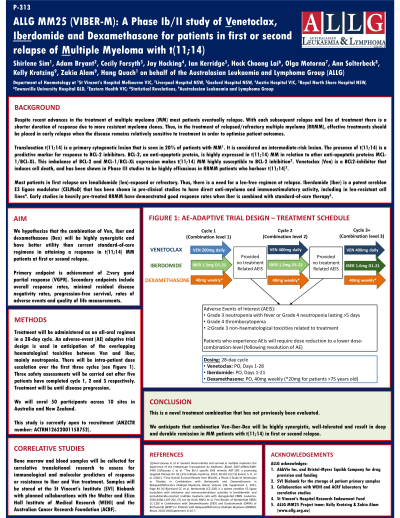
Methods: Treatment will be administered as an all oral regimen in a 28-day cycle: Ven on Days 1-28; Iber on Days 1-21; and weekly Dex. An adverse-event adapted trial design is used in anticipation of overlapping haematological toxicities between Ven and Iber, mainly neutropenia. There will be intra-patient dose escalation over the first three cycles; if there is no Grade 3 neutropenia with fever or Grade 4 neutropenia lasting more than 5 days, Grade 4 thrombocytopenia or ≥Grade 3 treatment-related non-haematological toxicities, doses will be escalated (Cycle 1: Iber 1.3mg/Ven 200mg; Cycle 2: Iber 1.3mg/Ven 400mg; Cycle 3 onwards: Iber 1.6mg/Ven 400mg). Three safety assessments will be carried out after five patients have completed cycle 1, 2 and 3 respectively. Treatment will be until disease progression. Primary endpoint is achievement of very good partial response or better.
Total study duration will be 4.5 years, with recruitment over 24 months, median expected time on treatment of 24 months, and follow up until 6 months after the last patient has had their last dose of treatment. This research is a cooperative trial group study lead by the Australasian Leukaemia and Lymphoma Group (ALLG), as ALLG MM25. This study is supported by AbbVie Inc. and Bristol-Myers Squibb Company.
Results: NA
Conclusions: We anticipate that combination Ven-Iber-Dex will be well tolerated and result in deep and durable remission in MM patients with t(11;14) in first or second relapse.
In the current era where lenalidomide (len) maintenance is used in first line, there is a need for a len-free regimen at relapse. Iberdomide is a potent cereblon E3 ligase modulator (CELMod) that has been shown in pre-clinical studies to have direct anti-myeloma and immunostimulatory activity, including in len- and pomalidomide-resistant cell lines. Early studies in heavily pre-treated RRMM have demonstrated good response rates when iberdomide is combined with standard-of-care therapy.
We hypothesize that the combination of Ven, iberdomide (Iber) and dexamethasone (Dex) will be highly synergistic and have better utility in rescuing MM patients with t(11;14) at first or second relapse.
Methods: Treatment will be administered as an all oral regimen in a 28-day cycle: Ven on Days 1-28; Iber on Days 1-21; and weekly Dex. An adverse-event adapted trial design is used in anticipation of overlapping haematological toxicities between Ven and Iber, mainly neutropenia. There will be intra-patient dose escalation over the first three cycles; if there is no Grade 3 neutropenia with fever or Grade 4 neutropenia lasting more than 5 days, Grade 4 thrombocytopenia or ≥Grade 3 treatment-related non-haematological toxicities, doses will be escalated (Cycle 1: Iber 1.3mg/Ven 200mg; Cycle 2: Iber 1.3mg/Ven 400mg; Cycle 3 onwards: Iber 1.6mg/Ven 400mg). Three safety assessments will be carried out after five patients have completed cycle 1, 2 and 3 respectively. Treatment will be until disease progression. Primary endpoint is achievement of very good partial response or better.
Total study duration will be 4.5 years, with recruitment over 24 months, median expected time on treatment of 24 months, and follow up until 6 months after the last patient has had their last dose of treatment. This research is a cooperative trial group study lead by the Australasian Leukaemia and Lymphoma Group (ALLG), as ALLG MM25. This study is supported by AbbVie Inc. and Bristol-Myers Squibb Company.
Results: NA
Conclusions: We anticipate that combination Ven-Iber-Dex will be well tolerated and result in deep and durable remission in MM patients with t(11;14) in first or second relapse.
