Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-314: Bendamustine Salvage for Relapsed – Refractory Multiple Myeloma: A retrospective analysis of outcomes in heavily pretreated patients.
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Aakanksha Singh, MD, DrNB (she/her/hers)
Trainee Physician
Rajiv Gandhi Cancer institute and Research Center
new delhi, Delhi, India
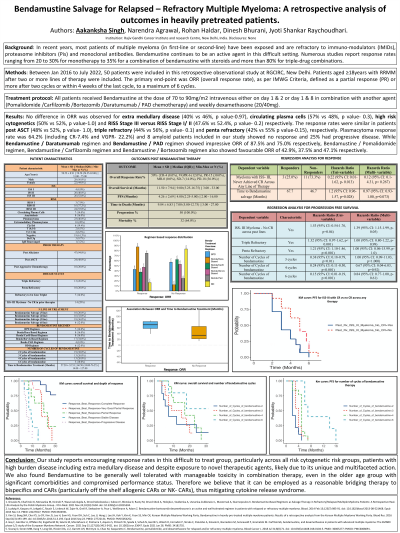
Introduction: Multiple myeloma in first-line or second-line setting are exposed and hence become refractory to IMIDs, PIs and monoclonal antibodies. The response rates of bendamustine in relapsed/ refractory multiple myeloma ranged from 20 to 30% for monotherapy to >80% for triple-drug combinations.
Methods: From Jan 2016 to July 2022, 50 patients of RRMM after two or more lines of therapy were included. ORR (overall response rate) defined as a partial response or more after two cycles to a maximum of 6 cycles. Bendamustine in combination with Pomalidomide/Carfilzomib/Bortezomib/Daratumumab/PAD chemotherapy and dexamethasone was given.
Results: All patients had prior PI (including Carfilzomib) and IMid (including Pomalidomide) exposure. 28.0% patients had prior Daratumumab exposure. 48.0% patients had prior ASCT, 26.0% patients were Triple Refractory and 20.0% were Penta-Refractory. 46.0% patients had Plasmacytoma (Paraskeletal- 13, Extramedullary-10), 14% Circulating plasma cells, 16% Secondary amyloidosis and 22% High Risk cytogenetics. In total, 25 (50%) patients responded and included: CR-8.0%, VGPR-12.0% and PR-30.0%. No difference in ORR observed for presence or absence of Extra Medullary Disease (40% vs 46%), circulating plasma cells (57 % vs 48%), high risk cytogenetics (50% vs 52%) and RISS Stage III vs RISS Stage I/II (47.6% vs 52.4%) respectively. The response rates were similar in patients who relapsed after ASCT versus not (48% vs 52%), triple refractory (44% vs 56%) and penta refractory (42% vs 55%), respectively with p value>0.05. While Bendamustine/ Daratumumab and Bendamustine/ PAD showed impressive ORR of 87.5% and 75.0% respectively, the Bendamustine/ Pomalidomide, Bendamustine/ Carfilzomib and Bendamustine/ Bortezomib also showed an ORR of 42.9%, 37.5% and 47.1% respectively. Bendamustine/ Dexamethasone had a dismal ORR-16.7%. Patients < CR in prior lines of therapy had an inferior ORR (HR-0.12, 95% CI: 0.01 to 4.31, p- 0.02). Responders had a longer time to bendamustine therapy (67.7 months) vs non responders (46.9 months) (HR-1.8, 95% CI: 0.96-2.38, p-0.028). Best response rates were documented post >/=3 cycles of chemotherapy (HR 1.29, 95% CI 1.01 – 1.80, p- 0.046). At a median follow-up of 11.5 months, median PFS and OS were 4 (95% CI: 2.25-5.00) months and 9.00 (95% CI: 5.25- not reached) months respectively. 32 (64%) of patients died on follow up. Patients with < CR in all prior lines of therapy had inferior OS, HR 1.39 (95% CI: 1.15-2.00, p=0.050) and PFS (HR 1.39, 95% CI: 1.15-1.99, p-0.050). Triple refractory myeloma (HR 1.32, 95% CI: 1.17-1.62, p-0.001) and Penta refractory (HR 1.21, 95% CI: 1.10-1.46, p< 0.001) had an inferior PFS. 8% patients had Grade 3/4 hematological toxicity requiring dose reduction.
Conclusions: Bendamustine showed encouraging responses across all risk groups, high burden disease and heavily pretreated patients post exposure to novel agents, making an excellent bridging therapy to bispecifics, off the shelf allogenic CARs and NK- CARs.
Methods: From Jan 2016 to July 2022, 50 patients of RRMM after two or more lines of therapy were included. ORR (overall response rate) defined as a partial response or more after two cycles to a maximum of 6 cycles. Bendamustine in combination with Pomalidomide/Carfilzomib/Bortezomib/Daratumumab/PAD chemotherapy and dexamethasone was given.
Results: All patients had prior PI (including Carfilzomib) and IMid (including Pomalidomide) exposure. 28.0% patients had prior Daratumumab exposure. 48.0% patients had prior ASCT, 26.0% patients were Triple Refractory and 20.0% were Penta-Refractory. 46.0% patients had Plasmacytoma (Paraskeletal- 13, Extramedullary-10), 14% Circulating plasma cells, 16% Secondary amyloidosis and 22% High Risk cytogenetics. In total, 25 (50%) patients responded and included: CR-8.0%, VGPR-12.0% and PR-30.0%. No difference in ORR observed for presence or absence of Extra Medullary Disease (40% vs 46%), circulating plasma cells (57 % vs 48%), high risk cytogenetics (50% vs 52%) and RISS Stage III vs RISS Stage I/II (47.6% vs 52.4%) respectively. The response rates were similar in patients who relapsed after ASCT versus not (48% vs 52%), triple refractory (44% vs 56%) and penta refractory (42% vs 55%), respectively with p value>0.05. While Bendamustine/ Daratumumab and Bendamustine/ PAD showed impressive ORR of 87.5% and 75.0% respectively, the Bendamustine/ Pomalidomide, Bendamustine/ Carfilzomib and Bendamustine/ Bortezomib also showed an ORR of 42.9%, 37.5% and 47.1% respectively. Bendamustine/ Dexamethasone had a dismal ORR-16.7%. Patients < CR in prior lines of therapy had an inferior ORR (HR-0.12, 95% CI: 0.01 to 4.31, p- 0.02). Responders had a longer time to bendamustine therapy (67.7 months) vs non responders (46.9 months) (HR-1.8, 95% CI: 0.96-2.38, p-0.028). Best response rates were documented post >/=3 cycles of chemotherapy (HR 1.29, 95% CI 1.01 – 1.80, p- 0.046). At a median follow-up of 11.5 months, median PFS and OS were 4 (95% CI: 2.25-5.00) months and 9.00 (95% CI: 5.25- not reached) months respectively. 32 (64%) of patients died on follow up. Patients with < CR in all prior lines of therapy had inferior OS, HR 1.39 (95% CI: 1.15-2.00, p=0.050) and PFS (HR 1.39, 95% CI: 1.15-1.99, p-0.050). Triple refractory myeloma (HR 1.32, 95% CI: 1.17-1.62, p-0.001) and Penta refractory (HR 1.21, 95% CI: 1.10-1.46, p< 0.001) had an inferior PFS. 8% patients had Grade 3/4 hematological toxicity requiring dose reduction.
Conclusions: Bendamustine showed encouraging responses across all risk groups, high burden disease and heavily pretreated patients post exposure to novel agents, making an excellent bridging therapy to bispecifics, off the shelf allogenic CARs and NK- CARs.
