Cellular and T cell engager Immunotherapy
Poster Session 1
P-037: BMS-986393 (CC-95266), a G protein-coupled receptor class C group 5 member D (GPRC5D)-targeted CAR T-cell therapy for relapsed/refractory multiple myeloma (RRMM): results from a phase 1 study
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Omar Nadeem, MD
Clinical Director
Dana-Farber Cancer Institute
Boston, Massachusetts, United States
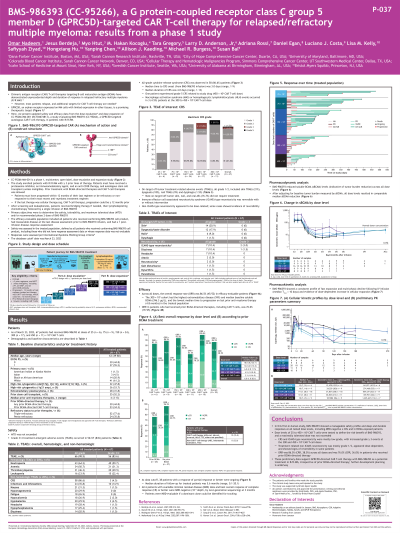
Introduction: Chimeric antigen receptor (CAR) T-cell therapies targeting B cell maturation antigen (BCMA) have shown deep response in RRMM but new targets are needed as most patients (pts) relapse. GPRC5D, an orphan receptor expressed on MM cells with limited expression in other tissues, is a promising therapeutic target for MM. We present safety and efficacy from the Part A dose escalation of CC-95266-MM-001 (NCT04674813), a phase 1, first-in-human, multicenter open-label study of BMS-986393 (CC-95266), a GPRC5D-targeted autologous CAR T-cell therapy, in pts with RRMM.
Methods: Part A included pts with ≥3 prior lines of therapy, with prior BCMA-directed and CAR T-cell therapies allowed. After leukapheresis and lymphodepletion, pts had a single infusion of BMS-986393. Safety, maximum tolerated dose (MTD), and/or recommended phase 2 dose were primary objectives.
Results: As of 7 Sept 2022, 33/40 enrolled pts received BMS-986393 at doses of 25, 75, 150, 300, and 450 × 10⁶ CAR T cells. Of these, 48% had high-risk cytogenetics and 45% had extramedullary plasmacytomas. Eighteen (55%) pts had received prior BCMA-targeted therapies, including BCMA-directed CAR T-cell therapy (13 pts); 24% had penta-refractory MM.
Grade (G) 3/4 treatment-emergent adverse events (TEAEs) occurred in 24/33 (73%) pts; most frequently neutropenia (61%), anemia (21%) and thrombocytopenia (21%). On-target off-tumor TEAEs, all G1, included skin TEAEs (30%), dysgeusia (15%), nail TEAEs (9%) and dysphagia (3%).
Dose-limiting toxicities of prolonged (out to day 42) G4 neutropenia and/or thrombocytopenia occurred in 2 pts; MTD was not exceeded. Cytokine release syndrome (CRS) occurred in 21/33 pts (19 G1/2; 2 G3). Immune effector cell-associated neurotoxicity syndrome (ICANS)–type neurotoxicity occurred in 2 pts and was low-grade and reversible with steroid treatment.
Overall response rate was 89% (17/19) in efficacy-evaluable pts, including 7/9 pts with prior BCMA-directed therapies including CAR T cells. Median follow-up for treated pts was 3.1 mo (range, 0.1–15.5). At data cutoff, 15/17 pts with a response were ongoing.
All 4 pts with available minimal residual disease (MRD) data and best overall response of complete response (CR) were MRD-negative (10⁻⁵ depth) at 3 mo. BMS-986393 reduced soluble BCMA levels across all dose levels; BMS-986393 exposure showed dose-dependence.
Conclusions: As of data cutoff, dose escalation of BMS-986393 from 25–450 × 10⁶ CAR T cells did not exceed MTD. CRS was mostly G1/2. ICANS-type neurotoxicity was infrequent, low-grade and reversible. A minority of pts had on-target off-tumor TEAEs, all G1. BMS-986393 showed durable responses and efficacy at all tested dose levels, including MRD-negative CRs and in pts previously exposed to BCMA-directed therapies. These preliminary data support GPRC5D-directed CAR T-cell therapy with BMS-986393 for treating RRMM, irrespective of prior BCMA-directed therapy. Part B dose expansion is underway. Updated data will be reported. Presented at EHA 2023. Abst S193.
Methods: Part A included pts with ≥3 prior lines of therapy, with prior BCMA-directed and CAR T-cell therapies allowed. After leukapheresis and lymphodepletion, pts had a single infusion of BMS-986393. Safety, maximum tolerated dose (MTD), and/or recommended phase 2 dose were primary objectives.
Results: As of 7 Sept 2022, 33/40 enrolled pts received BMS-986393 at doses of 25, 75, 150, 300, and 450 × 10⁶ CAR T cells. Of these, 48% had high-risk cytogenetics and 45% had extramedullary plasmacytomas. Eighteen (55%) pts had received prior BCMA-targeted therapies, including BCMA-directed CAR T-cell therapy (13 pts); 24% had penta-refractory MM.
Grade (G) 3/4 treatment-emergent adverse events (TEAEs) occurred in 24/33 (73%) pts; most frequently neutropenia (61%), anemia (21%) and thrombocytopenia (21%). On-target off-tumor TEAEs, all G1, included skin TEAEs (30%), dysgeusia (15%), nail TEAEs (9%) and dysphagia (3%).
Dose-limiting toxicities of prolonged (out to day 42) G4 neutropenia and/or thrombocytopenia occurred in 2 pts; MTD was not exceeded. Cytokine release syndrome (CRS) occurred in 21/33 pts (19 G1/2; 2 G3). Immune effector cell-associated neurotoxicity syndrome (ICANS)–type neurotoxicity occurred in 2 pts and was low-grade and reversible with steroid treatment.
Overall response rate was 89% (17/19) in efficacy-evaluable pts, including 7/9 pts with prior BCMA-directed therapies including CAR T cells. Median follow-up for treated pts was 3.1 mo (range, 0.1–15.5). At data cutoff, 15/17 pts with a response were ongoing.
All 4 pts with available minimal residual disease (MRD) data and best overall response of complete response (CR) were MRD-negative (10⁻⁵ depth) at 3 mo. BMS-986393 reduced soluble BCMA levels across all dose levels; BMS-986393 exposure showed dose-dependence.
Conclusions: As of data cutoff, dose escalation of BMS-986393 from 25–450 × 10⁶ CAR T cells did not exceed MTD. CRS was mostly G1/2. ICANS-type neurotoxicity was infrequent, low-grade and reversible. A minority of pts had on-target off-tumor TEAEs, all G1. BMS-986393 showed durable responses and efficacy at all tested dose levels, including MRD-negative CRs and in pts previously exposed to BCMA-directed therapies. These preliminary data support GPRC5D-directed CAR T-cell therapy with BMS-986393 for treating RRMM, irrespective of prior BCMA-directed therapy. Part B dose expansion is underway. Updated data will be reported. Presented at EHA 2023. Abst S193.
