Other plasma cell disorders
Poster Session 3
P-425: CARDIAC AL AMYLOIDOSIS EXPERIENCED IN THE LAST DECADE FROM A SINGLE CENTER
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Simge ERDEM, MD
Assistant Professor Dr.
Istanbul University Istanbul Faculty of Medicine, Department of Internal Medicine, Division of Hematology
Istanbul, Istanbul, Turkey
Introduction: Cardiac amyloidosis (CA) is rare and with poor prognosis. Light chain (AL) and transthyretin cardiac amyloidosis (ATTR) build up the main etiology. The presentation may be incidentally during different reasons evaluation or with signs and/or symptoms related to restrictive cardiomyopathy, heart failure, and /or conduction disease. In general, CA diagnosis is based on clinical suspicion and can be diagnosed noninvasively. Electrocardiogram (ECG), echocardiogram (ECHO), and cardiac magnetic resonance imaging (CMRI) are the often-used cardiac tests where the latter is less widely available. Early diagnosis of CA may modify the traditional poor biologic outcome in the era of the new drugs. Here we aimed to document the characteristics of CA cases as single-center experiences.
Methods: The institutional ECHO Laboratory automated system was screened retrospectively with the keyword of CA. The clinical characteristics were obtained from institutional follow-up charts in the Hematology department. All CA suspected cases were evaluated among paraproteinemia and plasma cell disorder. ECG and in some cases, CMRI were complimentary.
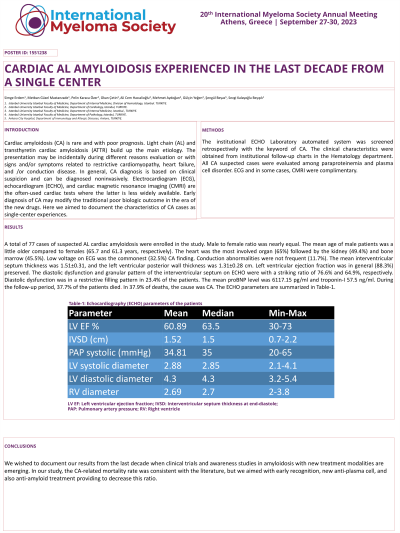
Results: A total of 77 cases of suspected AL cardiac amyloidosis were enrolled in the study. Male to female ratio was nearly equal. The mean age of male patients was a little older compared to females (65.7 and 61.3 years, respectively). The heart was the most involved organ (65%) followed by the kidney (49.4%) and bone marrow (45.5%). Low voltage on ECG was the commonest (32.5%) CA finding. Conduction abnormalities were not frequent (11.7%). The mean interventricular septum thickness was 1.51±0.31, and the left ventricular posterior wall thickness was 1.31±0.28 cm. Left ventricular ejection fraction was in general (88.3%) preserved. The diastolic dysfunction and granular pattern of the interventricular septum on ECHO were with a striking ratio of 76.6% and 64.9%, respectively. Diastolic dysfunction was in a restrictive filling pattern in 23.4% of the patients. The mean proBNP level was 6117.15 pg/ml and troponin-I 57.5 ng/ml. During the follow-up period, 37.7% of the patients died. In 37.9% of deaths, the cause was CA.
Conclusions: We wished to document our results from the last decade when clinical trials and awareness studies in amyloidosis with new treatment modalities are emerging. In our study, the CA-related mortality rate was consistent with the literature, but we aimed with early recognition, new anti-plasma cell, and also anti-amyloid treatment providing to decrease this ratio.
Keywords: AL amyloidosis, cardiac amyloidosis
Methods: The institutional ECHO Laboratory automated system was screened retrospectively with the keyword of CA. The clinical characteristics were obtained from institutional follow-up charts in the Hematology department. All CA suspected cases were evaluated among paraproteinemia and plasma cell disorder. ECG and in some cases, CMRI were complimentary.
Results: A total of 77 cases of suspected AL cardiac amyloidosis were enrolled in the study. Male to female ratio was nearly equal. The mean age of male patients was a little older compared to females (65.7 and 61.3 years, respectively). The heart was the most involved organ (65%) followed by the kidney (49.4%) and bone marrow (45.5%). Low voltage on ECG was the commonest (32.5%) CA finding. Conduction abnormalities were not frequent (11.7%). The mean interventricular septum thickness was 1.51±0.31, and the left ventricular posterior wall thickness was 1.31±0.28 cm. Left ventricular ejection fraction was in general (88.3%) preserved. The diastolic dysfunction and granular pattern of the interventricular septum on ECHO were with a striking ratio of 76.6% and 64.9%, respectively. Diastolic dysfunction was in a restrictive filling pattern in 23.4% of the patients. The mean proBNP level was 6117.15 pg/ml and troponin-I 57.5 ng/ml. During the follow-up period, 37.7% of the patients died. In 37.9% of deaths, the cause was CA.
Conclusions: We wished to document our results from the last decade when clinical trials and awareness studies in amyloidosis with new treatment modalities are emerging. In our study, the CA-related mortality rate was consistent with the literature, but we aimed with early recognition, new anti-plasma cell, and also anti-amyloid treatment providing to decrease this ratio.
Keywords: AL amyloidosis, cardiac amyloidosis
