MRD Assessment and role in Myeloma
Poster Session 1
P-087: Characterization of minimal residual disease (MRD) in patients with relapsed/refractory multiple myeloma treated with elranatamab: Analysis of MagnetisMM-3
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST
- CT
Cyrille Touzeau, MD;PhD
Professor of Hematology
CHU de Nantes, United States
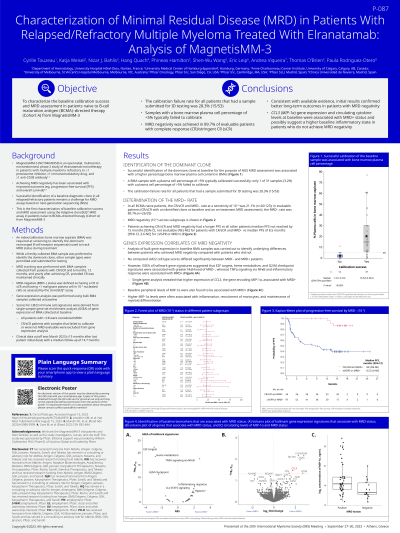
Introduction: MagnetisMM-3 (NCT04649359) is an open-label, multicenter, non-randomized, phase 2 study of elranatamab monotherapy in patients (pts) with multiple myeloma refractory to at least one proteasome inhibitor, one immunomodulatory drug and one anti-CD38 antibody. Achieving MRD negativity has been associated with improved outcomes (PFS, OS). However, successful identification of a baseline diagnostic clone in all relapsed refractory patients remains a challenge. This is the first characterization of baseline calibration success and MRD assessment in pts naïve to B-cell maturation antigen (BCMA)-directed therapy (Cohort A) from MagnetisMM-3.
Methods: An index/calibration bone marrow aspirate (BMA) was required at screening to identify the dominant rearranged B-cell receptor sequence(s) used to track MRD status during treatment. While a freshly collected BMA sample was preferred to identify the dominant clone, other sample types were permitted and submitted for testing. MRD tracking was performed with BMA samples collected at suspected CR/sCR and after 6 months, 12 months, and yearly after achieving CR. MRD negative status was defined as having a CR or sCR and having less than 1 malignant plasma cell in 10^-5 nucleated cells as assessed by the clonoSEQ assay. Bulk RNA-seq analysis was performed using BMA samples collected at screening. Clinical data cutoff was March 2023 (~15 months after last patient initial dose) with a median follow up of 14.7 months.
Results: Successful identification of the dominant clone at baseline for the purpose of NGS MRD assessment was primarily associated with a higher % BM plasma cell content. In all BCMA naïve patients the CR/sCR and MRD negative rate at a sensitivity of 10^-5 was 21.1% (n=26/123), and in evaluable patients (CR/sCR with an identified clone at baseline and an on-treatment MRD assessment) the MRD-negative rate was 89.7% (n=26/29). MRD-negativity was achieved across subgroups, however, as expected poor prognosis subgroups such as R-ISS 3, high-risk cytogenetics, presence of EMD or patients with penta-refractory disease achieved a lower MRD-negativity rate. Patients achieving CR/sCR and MRD-negativity had a longer PFS versus all other patients (median PFS not reached by 15 months [95% CI: NE, NE] for pts with CR/sCR and MRD negative vs median PFS of 8.5 months [95%, CI: 3.6, NE] for ≤VGPR or MRD positive).
Gene expression analysis of baseline BMA samples was carried out to identify underlying differences between patients that achieved MRD-negativity compared to patients that did not. These results and updated analyses including sustained MRD negativity will be presented.
Conclusions: MRD-negativity was achieved in 89.7% of evaluable patients. Consistent with available evidence, initial results confirmed better long-term outcomes in MRD-negative patients.
Methods: An index/calibration bone marrow aspirate (BMA) was required at screening to identify the dominant rearranged B-cell receptor sequence(s) used to track MRD status during treatment. While a freshly collected BMA sample was preferred to identify the dominant clone, other sample types were permitted and submitted for testing. MRD tracking was performed with BMA samples collected at suspected CR/sCR and after 6 months, 12 months, and yearly after achieving CR. MRD negative status was defined as having a CR or sCR and having less than 1 malignant plasma cell in 10^-5 nucleated cells as assessed by the clonoSEQ assay. Bulk RNA-seq analysis was performed using BMA samples collected at screening. Clinical data cutoff was March 2023 (~15 months after last patient initial dose) with a median follow up of 14.7 months.
Results: Successful identification of the dominant clone at baseline for the purpose of NGS MRD assessment was primarily associated with a higher % BM plasma cell content. In all BCMA naïve patients the CR/sCR and MRD negative rate at a sensitivity of 10^-5 was 21.1% (n=26/123), and in evaluable patients (CR/sCR with an identified clone at baseline and an on-treatment MRD assessment) the MRD-negative rate was 89.7% (n=26/29). MRD-negativity was achieved across subgroups, however, as expected poor prognosis subgroups such as R-ISS 3, high-risk cytogenetics, presence of EMD or patients with penta-refractory disease achieved a lower MRD-negativity rate. Patients achieving CR/sCR and MRD-negativity had a longer PFS versus all other patients (median PFS not reached by 15 months [95% CI: NE, NE] for pts with CR/sCR and MRD negative vs median PFS of 8.5 months [95%, CI: 3.6, NE] for ≤VGPR or MRD positive).
Gene expression analysis of baseline BMA samples was carried out to identify underlying differences between patients that achieved MRD-negativity compared to patients that did not. These results and updated analyses including sustained MRD negativity will be presented.
Conclusions: MRD-negativity was achieved in 89.7% of evaluable patients. Consistent with available evidence, initial results confirmed better long-term outcomes in MRD-negative patients.
