Plasma Cell Precursor Disorders
Poster Session 1
P-090: CLINICAL CHARACTERISTICS AND RISK OF PROGRESSION IN PATIENTS WITH MONOCLONAL GAMMOPATHY OF UNCERTAIN SIGNIFICANCE: LONG-TERM EXPERIENCE IN A SINGLE TERTIARY HOSPITAL.
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST
- EA
Elena Alejo
MD
Hospital Universitario de Salamanca
Salamanca, Castilla y Leon, Spain
Introduction: Monoclonal gammopathy of uncertain significance (MGUS) is a premalignant disease characterized by proliferation of aberrant plasma cells (aPC) with a high prevalence in the population over 50 years and annual risk of progression to multiple myeloma (MM) of 1%. Identification of factors associated to risk of progression is useful to individualize patient follow-up.
The aim was to identify potential risk factors at diagnosis in MGUS and to validate previously published progression-risk models.
Methods: An observational retrospective study was conducted including MGUS patients diagnosed at University Hospital of Salamanca between 1990 and 2022. MGUS was defined according to the criteria of the International Myeloma Working Group in 2014. Mayo Clinic and Burgos et al (MGUS-like phenotype) progression risk models were used.
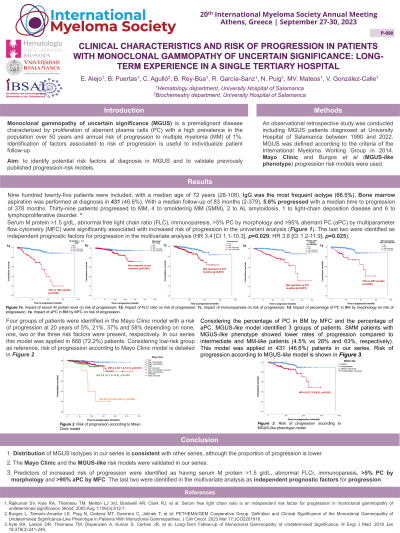
Results: The study is ongoing and, 700 patients have been reviewed so far, with a median age of 73 years (28-108). IgG was the most frequent isotype (67.6%), 11 were light-chain and 1 biclonal. Bone marrow aspiration at diagnosis was performed in 330 (47.1%) cases. Among those, median PC by morphology was 3% (0-9) and 6.7% had >95% aPC by multiparameter flow cytometry (MFC). When all variables were available, risk stratification according to the Mayo Clinic and the MGUS-like models were applied.
With a median follow-up of 95 months (2-379), 5.4% progressed with a median time to progression of 378 months. Thirty-one patients progressed to MM, 1 to AL amyloidosis, 1 to light-chain deposition disease and 5 to lymphoproliferative disorders.
In the univariant analysis, serum M protein>1.5 g/dL, abnormal free light chain ratio (FLCr), immunoparesia, >5% PC by morphology and >95% aPC by MFC were significantly associated with increased risk of progression, being the latter the only one identified as an independent prognostic factor for progression (Hazard ratio (HR) 4.6 [95% CI 1.3-17], p=0.020).
Mayo Clinic model was applied in 463 (66.1%) patients. Considering low-risk group as a reference, low-intermediate group had significantly higher risk of progression (HR 3.8 [95% CI, 1.1-14.1], p=0.046); same as high-intermediate (HR 7.2 [95% CI 1.9-27.5], p=0.003) and high risk (HR 34.5 [95% CI 6.9-171.5], p< 0.001). MGUS-like model was applied in 330 (47.1%) patients: intermediate phenotype was significantly associated with increased risk of progression as compared to MGUS-like (HR 6.4 [95% CI 2.5-16.4], p< 0.001).
Conclusions: 1. Distribution of MGUS isotypes in our series is consistent with other series, although the proportion of progression is lower.
2. The Mayo Clinic and the MGUS-like risk models were validated in our series.
3. Predictors of increased risk of progression were identified as having serum M protein>1.5 g/dL, abnormal FLCr, immunoparesia, >5% PC by morphology and >95% aPC by MFC. The latter was the only one identified as an independent prognostic factor for progression.
4. Analysis about entire series will be presented at the meeting.
The aim was to identify potential risk factors at diagnosis in MGUS and to validate previously published progression-risk models.
Methods: An observational retrospective study was conducted including MGUS patients diagnosed at University Hospital of Salamanca between 1990 and 2022. MGUS was defined according to the criteria of the International Myeloma Working Group in 2014. Mayo Clinic and Burgos et al (MGUS-like phenotype) progression risk models were used.
Results: The study is ongoing and, 700 patients have been reviewed so far, with a median age of 73 years (28-108). IgG was the most frequent isotype (67.6%), 11 were light-chain and 1 biclonal. Bone marrow aspiration at diagnosis was performed in 330 (47.1%) cases. Among those, median PC by morphology was 3% (0-9) and 6.7% had >95% aPC by multiparameter flow cytometry (MFC). When all variables were available, risk stratification according to the Mayo Clinic and the MGUS-like models were applied.
With a median follow-up of 95 months (2-379), 5.4% progressed with a median time to progression of 378 months. Thirty-one patients progressed to MM, 1 to AL amyloidosis, 1 to light-chain deposition disease and 5 to lymphoproliferative disorders.
In the univariant analysis, serum M protein>1.5 g/dL, abnormal free light chain ratio (FLCr), immunoparesia, >5% PC by morphology and >95% aPC by MFC were significantly associated with increased risk of progression, being the latter the only one identified as an independent prognostic factor for progression (Hazard ratio (HR) 4.6 [95% CI 1.3-17], p=0.020).
Mayo Clinic model was applied in 463 (66.1%) patients. Considering low-risk group as a reference, low-intermediate group had significantly higher risk of progression (HR 3.8 [95% CI, 1.1-14.1], p=0.046); same as high-intermediate (HR 7.2 [95% CI 1.9-27.5], p=0.003) and high risk (HR 34.5 [95% CI 6.9-171.5], p< 0.001). MGUS-like model was applied in 330 (47.1%) patients: intermediate phenotype was significantly associated with increased risk of progression as compared to MGUS-like (HR 6.4 [95% CI 2.5-16.4], p< 0.001).
Conclusions: 1. Distribution of MGUS isotypes in our series is consistent with other series, although the proportion of progression is lower.
2. The Mayo Clinic and the MGUS-like risk models were validated in our series.
3. Predictors of increased risk of progression were identified as having serum M protein>1.5 g/dL, abnormal FLCr, immunoparesia, >5% PC by morphology and >95% aPC by MFC. The latter was the only one identified as an independent prognostic factor for progression.
4. Analysis about entire series will be presented at the meeting.
