Cellular and T cell engager Immunotherapy
Poster Session 1
P-003: Clinical outcomes among multiple myeloma and lymphoma patients taking beta-blockers undergoing CAR-T therapy
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

Kristina A. Balandan, APRN, CNP (she/her/hers)
Nurse Practitioner
Mayo Clinic
Rochester, Minnesota, United States
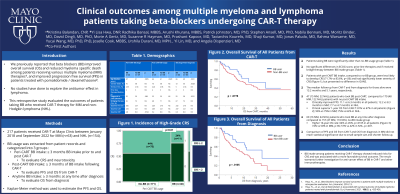
Introduction: The antineoplastic effect of beta blockers (BB) has been widely explored in solid tumors but understudied in hematologic malignancies. We previously reported that BB improved overall survival (OS) and reduced myeloma specific death among patients receiving various multiple myeloma (MM) therapies, and improved progression free survival (PFS) in patients treated with pomalidomide / dexamethasone. No studies have done to explore the antitumor effect in lymphoma. This retrospective study evaluated the outcomes of patients taking BB who received CAR-T therapy for MM and non-Hodgkin lymphoma (NHL).
Methods: We identified 217 patients received CAR-T at Mayo Clinic between January 2018 and September 2022 for MM (n=63) and NHL (n=154). BB usage was extracted from patient records. Peri-CART BB intake was defined as ≥ 3 months BB intake prior to and post CAR-T to evaluate CRS and neurotoxicity. Post-CART BB usage groups, defined as ≥ 3 months of BB intake following CAR-T, were compared to evaluate PFS and OS from CAR-T. OS from diagnosis was analyzed between patients with BB intake of ≥ 3 months at any time after diagnosis and no-BB usage group. Kaplan-Meier method was used to estimate the PFS and OS.
Results: During the peri-CAR-T period, there were 46 BB users and 171 non-BB users (median age of 67 versus 61 years, p=0.0005). Both groups had male predominance (70% in BB and 58% in no-BB patients). The time from diagnosis to CAR-T was not significantly different between the BB group and the non-BB group (55 months vs 30 months; p=0.88) nor were there significant differences between two groups in ECOG score, prior-line therapies and, if received, bridging therapy. The patients with peri-CART BB consumption, compared to no-BB group, were less likely to develop CRS (71.7% vs 83.6%, p=.06) and had significantly lower severity of CRS (grade ≥ 2: 23.9% vs 43.9%; p=0.01) but comparable ICANS rates. The median follow-up from CAR-T and from diagnosis for surviving patients was 13.2 months and 5.1 years, respectively. The 47 (15 MM, 32 NHL) patients who took BB post-CART, compared to 170 (48 MM, 122 NHL) patients with no post-CART BB intake, had superior PFS (11.1 vs 6.3 months in all patients; 12.2 vs 8.3 months in MM; 7.7 vs 4.7 months in NHL) and superior 1-year OS from CAR-T (81% vs 67% in all patients; 93% vs 79% in MM; 75% vs 62% in NHL). The 60 (16 MM, 44 NHL) patients who took BB at any time after diagnosis had higher 10-year OS from diagnosis than no-BB intake group (64% vs 45%, p=.0105 in all patients; 74% vs 50% in MM, p NS; 57% vs 42% in NHL, p=.007). Comparison of PFS and OS from CAR-T as well as OS from diagnosis in MM did not reach statistical significance due to small sample size and shorter follow up.
Conclusions: BB intake among patients receiving CAR-T therapy showed reduced risks for CRS and was associated with more favorable survival outcomes. The result warrants further investigation for anti-cancer effect of BB in CAR-T and other immunotherapies.
Methods: We identified 217 patients received CAR-T at Mayo Clinic between January 2018 and September 2022 for MM (n=63) and NHL (n=154). BB usage was extracted from patient records. Peri-CART BB intake was defined as ≥ 3 months BB intake prior to and post CAR-T to evaluate CRS and neurotoxicity. Post-CART BB usage groups, defined as ≥ 3 months of BB intake following CAR-T, were compared to evaluate PFS and OS from CAR-T. OS from diagnosis was analyzed between patients with BB intake of ≥ 3 months at any time after diagnosis and no-BB usage group. Kaplan-Meier method was used to estimate the PFS and OS.
Results: During the peri-CAR-T period, there were 46 BB users and 171 non-BB users (median age of 67 versus 61 years, p=0.0005). Both groups had male predominance (70% in BB and 58% in no-BB patients). The time from diagnosis to CAR-T was not significantly different between the BB group and the non-BB group (55 months vs 30 months; p=0.88) nor were there significant differences between two groups in ECOG score, prior-line therapies and, if received, bridging therapy. The patients with peri-CART BB consumption, compared to no-BB group, were less likely to develop CRS (71.7% vs 83.6%, p=.06) and had significantly lower severity of CRS (grade ≥ 2: 23.9% vs 43.9%; p=0.01) but comparable ICANS rates. The median follow-up from CAR-T and from diagnosis for surviving patients was 13.2 months and 5.1 years, respectively. The 47 (15 MM, 32 NHL) patients who took BB post-CART, compared to 170 (48 MM, 122 NHL) patients with no post-CART BB intake, had superior PFS (11.1 vs 6.3 months in all patients; 12.2 vs 8.3 months in MM; 7.7 vs 4.7 months in NHL) and superior 1-year OS from CAR-T (81% vs 67% in all patients; 93% vs 79% in MM; 75% vs 62% in NHL). The 60 (16 MM, 44 NHL) patients who took BB at any time after diagnosis had higher 10-year OS from diagnosis than no-BB intake group (64% vs 45%, p=.0105 in all patients; 74% vs 50% in MM, p NS; 57% vs 42% in NHL, p=.007). Comparison of PFS and OS from CAR-T as well as OS from diagnosis in MM did not reach statistical significance due to small sample size and shorter follow up.
Conclusions: BB intake among patients receiving CAR-T therapy showed reduced risks for CRS and was associated with more favorable survival outcomes. The result warrants further investigation for anti-cancer effect of BB in CAR-T and other immunotherapies.
