QoL and Patient-Reported Outcome and Supportive Care
Poster Session 3
P-486: Clinical significance of baseline body mass index and its trajectory during triplet induction therapy in newly diagnosed multiple myeloma
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Ross S. Firestone, MD/PhD (he/him/his)
Fellow - Hematology / Oncology
Memorial Sloan Kettering Cancer Center, New York City NY, USA
New York, New York, United States
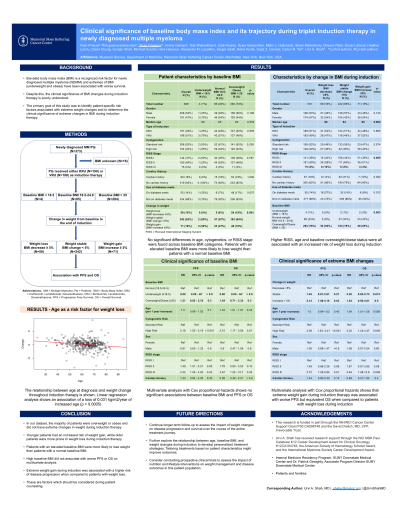
Introduction: Elevated body mass index (BMI) is a known risk factor for newly diagnosed multiple myeloma (NDMM); however, the prevalence and clinical significance of BMI changes (gain and loss) during induction therapy in NDMM has not been explored.
Methods: We conducted a retrospective study of 188 NDMM patients (pts) receiving induction therapy with carfilzomib, lenalidomide and dexamethasone (KRd) from 2016 to 2022 to determine the clinical significance of baseline BMI and trajectory during induction therapy. BMI was collected at baseline and at completion of induction therapy. Pts were divided into – underweight ( < 18.5), normal (18.5-24.9) and elevated BMI (≥ 25). Pts were also divided into – weight stable (BMI change < 5%), weight loss (BMI decrease ≥5%) and weight gain (BMI increase ≥5%) based on BMI change post induction from baseline. High risk cytogenetics was defined by the presence of +1q, del(17p), t(4;14), t(14;16) or t(14;20). Progression free survival (PFS) was defined as time from beginning induction therapy to disease progression or death. Univariate analysis was performed by unpaired two-sided t-tests or Cox proportional hazards for survival analyses. Multivariate analysis was performed using Cox proportional hazards regression analysis and model was adjusted for baseline BMI, cytogenetics, age, ECOG and ISS.
Results: Baseline BMI for pts were 1% underweight, 22% normal, 76% elevated, and 1% unknown. No differences in age, cytogenetics, or ISS stage were noted across baseline BMI categories. During induction, BMI for pts were 14% lost weight, 62% weight stable, and 21% gained weight. For pts with high-risk cytogenetics, 17% lost weight and 18% gained weight, whereas for pts with standard-risk cytogenetics, 13% lost weight and 25% gained weight.
Pts with weight gain had a lower median age than weight stable pts (58 years (y) vs 61y, p=0.073) and pts with weight loss had a significantly higher age than weight stable pts (66y vs 61y, p=0.008). On univariate analysis, PFS trended worse for pts with BMI >25 (median PFS NR for both groups, p=0.07). On multivariate analysis, pts with baseline BMI >25 (HR 3.2, p=0.05), high-risk cytogenetics (HR 2.0, p=0.04), and ISS stage 3 disease (HR 2.9, p=0.03) had worse PFS with no difference identified for patient age or ECOG.
No differences were observed in post-induction PFS when comparing weight stable pts to those gaining or losing weight (p=0.27).
Conclusions: Most pts in our dataset had an elevated BMI that was maintained during induction therapy. The increased risk for weight gain in younger pts and for weight loss in older pts should be considered for pt counseling, although this did not affect PFS. An elevated BMI tracks with inferior PFS. Data on a similar cohort of pts treated with bortezomib, lenalidomide, and dexamethasone along with long-term BMI trajectories post-induction from both cohorts will be presented at the meeting.
Methods: We conducted a retrospective study of 188 NDMM patients (pts) receiving induction therapy with carfilzomib, lenalidomide and dexamethasone (KRd) from 2016 to 2022 to determine the clinical significance of baseline BMI and trajectory during induction therapy. BMI was collected at baseline and at completion of induction therapy. Pts were divided into – underweight ( < 18.5), normal (18.5-24.9) and elevated BMI (≥ 25). Pts were also divided into – weight stable (BMI change < 5%), weight loss (BMI decrease ≥5%) and weight gain (BMI increase ≥5%) based on BMI change post induction from baseline. High risk cytogenetics was defined by the presence of +1q, del(17p), t(4;14), t(14;16) or t(14;20). Progression free survival (PFS) was defined as time from beginning induction therapy to disease progression or death. Univariate analysis was performed by unpaired two-sided t-tests or Cox proportional hazards for survival analyses. Multivariate analysis was performed using Cox proportional hazards regression analysis and model was adjusted for baseline BMI, cytogenetics, age, ECOG and ISS.
Results: Baseline BMI for pts were 1% underweight, 22% normal, 76% elevated, and 1% unknown. No differences in age, cytogenetics, or ISS stage were noted across baseline BMI categories. During induction, BMI for pts were 14% lost weight, 62% weight stable, and 21% gained weight. For pts with high-risk cytogenetics, 17% lost weight and 18% gained weight, whereas for pts with standard-risk cytogenetics, 13% lost weight and 25% gained weight.
Pts with weight gain had a lower median age than weight stable pts (58 years (y) vs 61y, p=0.073) and pts with weight loss had a significantly higher age than weight stable pts (66y vs 61y, p=0.008). On univariate analysis, PFS trended worse for pts with BMI >25 (median PFS NR for both groups, p=0.07). On multivariate analysis, pts with baseline BMI >25 (HR 3.2, p=0.05), high-risk cytogenetics (HR 2.0, p=0.04), and ISS stage 3 disease (HR 2.9, p=0.03) had worse PFS with no difference identified for patient age or ECOG.
No differences were observed in post-induction PFS when comparing weight stable pts to those gaining or losing weight (p=0.27).
Conclusions: Most pts in our dataset had an elevated BMI that was maintained during induction therapy. The increased risk for weight gain in younger pts and for weight loss in older pts should be considered for pt counseling, although this did not affect PFS. An elevated BMI tracks with inferior PFS. Data on a similar cohort of pts treated with bortezomib, lenalidomide, and dexamethasone along with long-term BMI trajectories post-induction from both cohorts will be presented at the meeting.
