Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-294: Comparative Effectiveness of Teclistamab vs Real-world Physician’s Choice of Therapy in the LocoMMotion and MoMMent Studies for Patients With Triple-class Exposed Relapsed/Refractory Multiple Myeloma
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

María-Victoria Mateos, MD, PhD
Professor
University Hospital of Salamanca/IBSAL/CIC/CIBERONC, Salamanca, Spain
Salamanca, Spain
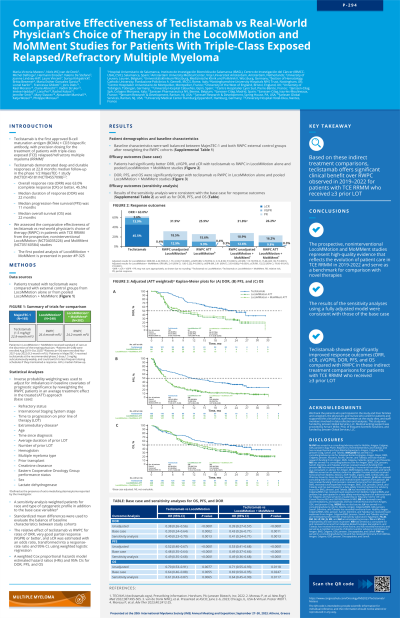
Introduction: Teclistamab, the only approved BCMA×CD3 bispecific antibody with a personalized, weight-based, and flexible dosing schedule for the treatment (tx) of triple-class exposed (TCE) relapsed/refractory multiple myeloma (RRMM), has shown promising efficacy in the phase 1/2 MajesTEC-1 study (NCT03145181/NCT04557098). As MajesTEC-1 is a single-arm study, we assessed the comparative effectiveness of teclistamab vs real-world physician’s choice of therapy (RWPC) in pts with TCE RRMM from the real-world, prospective, noninterventional studies, LocoMMotion (NCT04035226; enrolled Aug 2019–Oct 2020; clinical cut-off [CCO] Oct 27, 2022) and MoMMent (NCT05160584; enrolled Nov 2021–July 2022; CCO Oct 27, 2022). MoMMent was initiated as a complement to LocoMMotion to assess practice changes in recent years.
Methods: Pts treated with the recommended phase 2 dose of teclistamab (1.5 mg/kg tx doses) from MajesTEC-1 (N=165; CCO Jan 4, 2023) were compared with an external control arm from LocoMMotion alone (N=248) or from pooled LocoMMotion + MoMMent (N=302). Inverse probability of tx weighting estimating the average tx effect in the treated population was used to adjust for imbalances in baseline covariates of prognostic significance: refractory status, ISS stage, time to progression on prior line of therapy [LOT], extramedullary disease, number of prior LOTs, time since diagnosis, average duration of prior LOTs, age, hemoglobin, lactate dehydrogenase, creatinine clearance, ECOG performance status, gender, MM type, and prior transplant. Relative effect of teclistamab vs RWPC for rates of overall response (ORR), very good partial response or better (≥VGPR), and complete response or better (≥CR) was estimated with an odds ratio using weighted logistic regression transformed into a response-rate ratio (RR) and 95% CI. A weighted Cox proportional hazards model was used to estimate hazard ratios (HRs) and 95% CIs for duration of response (DOR), progression-free survival (PFS), and overall survival (OS).
Results: Baseline characteristics were well balanced between the 3 cohorts after reweighting external control arms. Pts treated with teclistamab had significantly improved outcomes vs RWPC in LocoMMotion: ORR (RR [95% CI], 2.32 [1.71–3.15]; P< 0.0001), ≥VGPR (RR, 5.60 [3.64–8.62]; P< 0.0001), ≥CR (RR, 183.80 [14.89–2268.30]; P< 0.0001), DOR (HR, 0.35 [0.21–0.56]; P< 0.0001), PFS (HR, 0.47 [0.35–0.64]; P< 0.0001), and OS (HR, 0.64 [0.47–0.88]; P=0.0051). Teclistamab vs RWPC in LocoMMotion + MoMMent also had significantly improved outcomes: ORR (RR [95% CI], 2.38 [1.78–3.19]; P< 0.0001), ≥VGPR (RR, 6.02 [4.00–9.08]; P< 0.0001), ≥CR (RR, 178.55 [18.88–1688.40]; P< 0.0001), DOR (HR, 0.38 [0.23–0.63]; P=0.0002), PFS (HR, 0.48 [0.35–0.65]; P< 0.0001), and OS (HR, 0.67 [0.49–0.91]; P=0.0117).
Conclusions: Teclistamab demonstrated significantly improved effectiveness over RWPC in LocoMMotion alone and pooled LocoMMotion + MoMMent, emphasizing its clinical benefit as a highly effective tx for pts with TCE RRMM.
Methods: Pts treated with the recommended phase 2 dose of teclistamab (1.5 mg/kg tx doses) from MajesTEC-1 (N=165; CCO Jan 4, 2023) were compared with an external control arm from LocoMMotion alone (N=248) or from pooled LocoMMotion + MoMMent (N=302). Inverse probability of tx weighting estimating the average tx effect in the treated population was used to adjust for imbalances in baseline covariates of prognostic significance: refractory status, ISS stage, time to progression on prior line of therapy [LOT], extramedullary disease, number of prior LOTs, time since diagnosis, average duration of prior LOTs, age, hemoglobin, lactate dehydrogenase, creatinine clearance, ECOG performance status, gender, MM type, and prior transplant. Relative effect of teclistamab vs RWPC for rates of overall response (ORR), very good partial response or better (≥VGPR), and complete response or better (≥CR) was estimated with an odds ratio using weighted logistic regression transformed into a response-rate ratio (RR) and 95% CI. A weighted Cox proportional hazards model was used to estimate hazard ratios (HRs) and 95% CIs for duration of response (DOR), progression-free survival (PFS), and overall survival (OS).
Results: Baseline characteristics were well balanced between the 3 cohorts after reweighting external control arms. Pts treated with teclistamab had significantly improved outcomes vs RWPC in LocoMMotion: ORR (RR [95% CI], 2.32 [1.71–3.15]; P< 0.0001), ≥VGPR (RR, 5.60 [3.64–8.62]; P< 0.0001), ≥CR (RR, 183.80 [14.89–2268.30]; P< 0.0001), DOR (HR, 0.35 [0.21–0.56]; P< 0.0001), PFS (HR, 0.47 [0.35–0.64]; P< 0.0001), and OS (HR, 0.64 [0.47–0.88]; P=0.0051). Teclistamab vs RWPC in LocoMMotion + MoMMent also had significantly improved outcomes: ORR (RR [95% CI], 2.38 [1.78–3.19]; P< 0.0001), ≥VGPR (RR, 6.02 [4.00–9.08]; P< 0.0001), ≥CR (RR, 178.55 [18.88–1688.40]; P< 0.0001), DOR (HR, 0.38 [0.23–0.63]; P=0.0002), PFS (HR, 0.48 [0.35–0.65]; P< 0.0001), and OS (HR, 0.67 [0.49–0.91]; P=0.0117).
Conclusions: Teclistamab demonstrated significantly improved effectiveness over RWPC in LocoMMotion alone and pooled LocoMMotion + MoMMent, emphasizing its clinical benefit as a highly effective tx for pts with TCE RRMM.
