Treatment of Newly Diagnosed Myeloma - Transplant Eligible
Poster Session 1
P-151: Demographic and Clinical Characteristics of Multiple Myeloma Patients in a Tertiary Cancer institute of India
Wednesday, September 27, 2023
1:30 PM - 2:30 PM EEST

DHYEY RAJKUMAR MISHRA (he/him/his)
3RD YEAR MBBS STUDENT
SETH GS MEDICAL COLLEGE AND KEM HOSPITAL, MUMBAI
KALYAN, Maharashtra, India
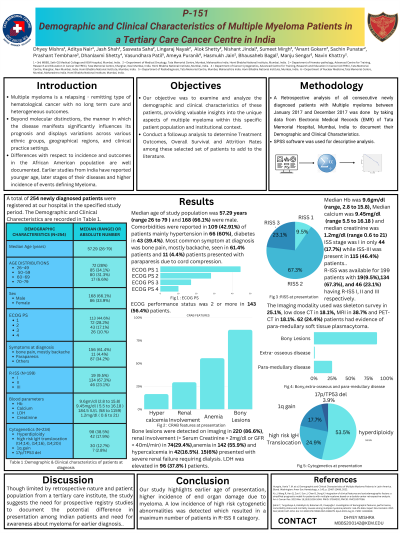
Introduction: Multiple myeloma is a relapsing remitting type of hematological cancer with no long term cure and heterogeneous outcomes. Presenting features impacts outcomes and varies across different ethnic and geographic regions. Differences with respect to incidence and outcomes in the African American population are well documented. Earlier studies from India have reported young age, late stages of the diseases and high incidence of myeloma defining events. We looked at consecutive cohort of patients with newly diagnosed myeloma over a year at a tertiary cancer institute to see the demographic and presenting characteristics.
Methods: We did a retrospective analysis of all consecutive newly diagnosed patients with Multiple myeloma between January 2017 and December 2017. Data was collected from the electronic medical record. SPSSV22 was used for descriptive analysis.
Results: A total of 254 newly diagnosed patients were registered at our hospital in the specified study period. Median age of study population was 57.2 years (range 26 to 79) and 168 (66.1%) were male. Comorbidities were reported in 109(42.9%) patients, mainly hypertension in 66 (60%),diabetes in 43 (39.4%). ECOG performance status was 2 or more in 143 (56.4%) patients. Most common symptom at diagnosis was bone pain, mostly backache, seen in 61.4% patients and 11 (4.4%) patients presented with paraparesis due to cord compression. Bone lesions were detected on imaging in 220 (86.6%), renal involvement in 74 (29.4%), anemia in 142 (55.9%) and hypercalcemia in 42 (16.5%). Fifteen (6%) presented with severe renal failure requiring dialysis. Median Hb was 9.6gm/dl (range 2.8 to 15.8), Median calcium was 9.45mg/dl (range 5.5 to 16.18 ) and median creatinine was 1.2mg/dl (range 0.6 to 21). The Imaging modality used was skeleton survey in 25.1%, low dose CT in 18.1%, MRI in 38.7% and PET-CT in 18.1%. 62(24.4%) patients had evidence of paramedullary soft tissue plasmacytoma. ISS stage was I in only 44 (17.7%) while ISS-III was present in 115 (46.4%) patients. LDH was elevated in 96 (37.8%) patients. Cytogenetics revealed hyperdiploidy in 98 out of 234 tested for same (38.5%) and high risk IgH translocation (t(4;14), (14;16), (14;20)) was reported in 42 (17.9%) patients while 1q gain was present in 30 (12.7%) patients. 17p/TP53 del was detected in 7(2.8%) patients. R-ISS was available for 199 patients with 19 (9.5%),134 (67.3%), and 46 (23.1%) having R-ISS I, II and III respectively.
Conclusions: Our study highlights earlier age of presentation, higher incidence of end organ damage due to myeloma. A low incidence of high risk cytogenetic abnormalities was detected which resulted in a maximum number of patients in R-ISS II category. Though limited by retrospective nature and patient population from a tertiary care institute, the study suggests the need for prospective registry studies to document the potential difference in presentation among Indian patients and need for awareness about myeloma for early diagnosis.
Methods: We did a retrospective analysis of all consecutive newly diagnosed patients with Multiple myeloma between January 2017 and December 2017. Data was collected from the electronic medical record. SPSSV22 was used for descriptive analysis.
Results: A total of 254 newly diagnosed patients were registered at our hospital in the specified study period. Median age of study population was 57.2 years (range 26 to 79) and 168 (66.1%) were male. Comorbidities were reported in 109(42.9%) patients, mainly hypertension in 66 (60%),diabetes in 43 (39.4%). ECOG performance status was 2 or more in 143 (56.4%) patients. Most common symptom at diagnosis was bone pain, mostly backache, seen in 61.4% patients and 11 (4.4%) patients presented with paraparesis due to cord compression. Bone lesions were detected on imaging in 220 (86.6%), renal involvement in 74 (29.4%), anemia in 142 (55.9%) and hypercalcemia in 42 (16.5%). Fifteen (6%) presented with severe renal failure requiring dialysis. Median Hb was 9.6gm/dl (range 2.8 to 15.8), Median calcium was 9.45mg/dl (range 5.5 to 16.18 ) and median creatinine was 1.2mg/dl (range 0.6 to 21). The Imaging modality used was skeleton survey in 25.1%, low dose CT in 18.1%, MRI in 38.7% and PET-CT in 18.1%. 62(24.4%) patients had evidence of paramedullary soft tissue plasmacytoma. ISS stage was I in only 44 (17.7%) while ISS-III was present in 115 (46.4%) patients. LDH was elevated in 96 (37.8%) patients. Cytogenetics revealed hyperdiploidy in 98 out of 234 tested for same (38.5%) and high risk IgH translocation (t(4;14), (14;16), (14;20)) was reported in 42 (17.9%) patients while 1q gain was present in 30 (12.7%) patients. 17p/TP53 del was detected in 7(2.8%) patients. R-ISS was available for 199 patients with 19 (9.5%),134 (67.3%), and 46 (23.1%) having R-ISS I, II and III respectively.
Conclusions: Our study highlights earlier age of presentation, higher incidence of end organ damage due to myeloma. A low incidence of high risk cytogenetic abnormalities was detected which resulted in a maximum number of patients in R-ISS II category. Though limited by retrospective nature and patient population from a tertiary care institute, the study suggests the need for prospective registry studies to document the potential difference in presentation among Indian patients and need for awareness about myeloma for early diagnosis.
