Other plasma cell disorders
Poster Session 3
P-419: Demographics, Clinical Features and Treatment Outcomes of Waldenstrom Macroglobulinemia from a Tertiary Care Cancer Centre in India.
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Bhausaheb Bagal, MD (he/him/his)
Professor
Department of Medical Oncology, Tata Memorial Centre
Mumbai, Maharashtra, India
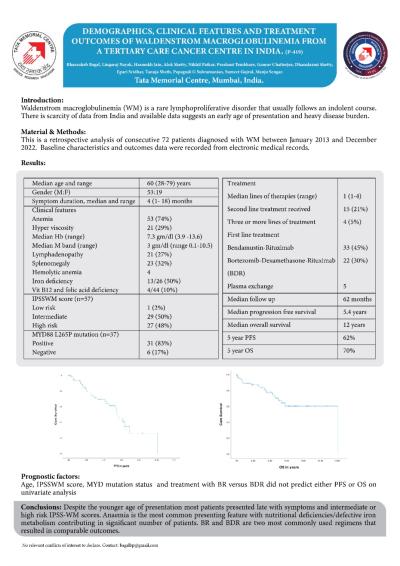
Introduction: Waldenstrom macroglobulinemia (WM) is a rare lymphoproliferative disorder that usually follows an indolent course. There is scarcity of data from Indian patients and available data suggest an early age of presentation, diagnosis with heavy disease burden.
Methods: All consecutive patients diagnosed with WM between January 2013 and December 2022 were included in this analysis. The progression free survival (PFS) was calculated from date of treatment to disease progression or death and overall survival (OS) was defined as the duration from the diagnosis of WM to the date of death or last follow-up.
Results: Seventy two patients were enrolled in this analysis and 57 patients were male ( 79 %) with a median age of 60 years (range 28-79 years). Most common presenting symptom was anaemia in 53 (74%), 4 had hemolytic anaemia, 13 out of 26 patients who had iron studies available showed concomitant iron deficiency anaemia and 4 of 44 patients tested had either vit B12 or folic acid deficiency. Symptoms of hyperviscosity were recorded in 21 (29%) patients out of which 5 patients underwent plasmapheresis. Symptom duration ranged from less than 1 month to 18 months with a median time of 4 months before diagnosis. The median haemoglobin at presentation was 7.3 gm/dl (range 3.9 -13.6) and median M band concentration was 3 gm/dl (range 0.1-10.5). Lymphadenopathy was recorded in 21 (27%) patients while splenomegaly was present in 23 (32%) patients. The International Prognostic Scoring System for WM (IPSSWM) at diagnosis was available for 57 patients with 29 (40%) in intermediate risk group and 27 (37.5%) in high risk group while only one patient in low risk group. Thirty seven patients had undergone MYD88 testing, out of which 31 (83%) patients were tested positive for MYD88 L265P mutation. Bendamustin-Rituximab was the most commonly used regimen followed by Bortezomib-Dexamethasome-Rituxima (BDR) in 33 (45%) and 22 (30%) respectively. Median lines of therapy received was one range (range 1-4) with second-line therapies administered to 15 (21%) patients while third or more lines were administered only in 4 (5%) patients.
Over a median follow up period of 62 months, 28 patients have progressed with a median PFS of 5.4 months and 2 year and 5 years PFS of 80 and 62% respectively. Twenty patients have died with an estimated median OS of 12 years and 2 years and 5 year OS of 87 % and 70 % respectively. None of the variables tested including IPSS-WM scores, therapy received and MYD88 mutation status were significantly associated with PFS and OS.
Conclusions: Despite the younger age of presentation most patients presented late with symptoms and intermediate or high risk IPSS-WM scores. Anaemia is the most common presentation with nutritional deficiencies/defective iron metabolism contributing in a significant number of patients. BR and BDR are two most commonly used regimens that result in comparable outcomes.
Methods: All consecutive patients diagnosed with WM between January 2013 and December 2022 were included in this analysis. The progression free survival (PFS) was calculated from date of treatment to disease progression or death and overall survival (OS) was defined as the duration from the diagnosis of WM to the date of death or last follow-up.
Results: Seventy two patients were enrolled in this analysis and 57 patients were male ( 79 %) with a median age of 60 years (range 28-79 years). Most common presenting symptom was anaemia in 53 (74%), 4 had hemolytic anaemia, 13 out of 26 patients who had iron studies available showed concomitant iron deficiency anaemia and 4 of 44 patients tested had either vit B12 or folic acid deficiency. Symptoms of hyperviscosity were recorded in 21 (29%) patients out of which 5 patients underwent plasmapheresis. Symptom duration ranged from less than 1 month to 18 months with a median time of 4 months before diagnosis. The median haemoglobin at presentation was 7.3 gm/dl (range 3.9 -13.6) and median M band concentration was 3 gm/dl (range 0.1-10.5). Lymphadenopathy was recorded in 21 (27%) patients while splenomegaly was present in 23 (32%) patients. The International Prognostic Scoring System for WM (IPSSWM) at diagnosis was available for 57 patients with 29 (40%) in intermediate risk group and 27 (37.5%) in high risk group while only one patient in low risk group. Thirty seven patients had undergone MYD88 testing, out of which 31 (83%) patients were tested positive for MYD88 L265P mutation. Bendamustin-Rituximab was the most commonly used regimen followed by Bortezomib-Dexamethasome-Rituxima (BDR) in 33 (45%) and 22 (30%) respectively. Median lines of therapy received was one range (range 1-4) with second-line therapies administered to 15 (21%) patients while third or more lines were administered only in 4 (5%) patients.
Over a median follow up period of 62 months, 28 patients have progressed with a median PFS of 5.4 months and 2 year and 5 years PFS of 80 and 62% respectively. Twenty patients have died with an estimated median OS of 12 years and 2 years and 5 year OS of 87 % and 70 % respectively. None of the variables tested including IPSS-WM scores, therapy received and MYD88 mutation status were significantly associated with PFS and OS.
Conclusions: Despite the younger age of presentation most patients presented late with symptoms and intermediate or high risk IPSS-WM scores. Anaemia is the most common presentation with nutritional deficiencies/defective iron metabolism contributing in a significant number of patients. BR and BDR are two most commonly used regimens that result in comparable outcomes.
