Myeloma Microenvironment and immune profiling
Poster Session 3
P-408: Differential peripheral cytokine profile and tumor microenvironment in patients with or without a history of BCMA-directed therapy prior to elranatamab: Analysis of MagnetisMM-3
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST
.jpg)
Paula Rodríguez-Otero, MD, PhD (she/her/hers)
Associate Professor
Clínica Universidad de Navarra, CIMA, CIBERONC, IDISNA, Pamplona, Spain
Pamplona, Navarra, Spain
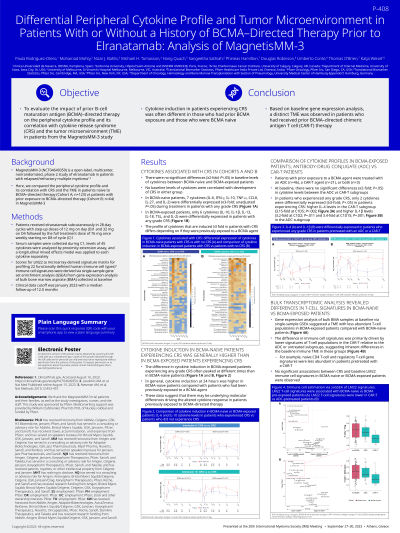
Introduction: MagnetisMM-3 (NCT04649359) is a phase 2 study of elranatamab in patients (pts) with relapsed/refractory multiple myeloma. Here, we compare the peripheral cytokine profile, its correlation with cytokine release syndrome (CRS) and tumor microenvironment (TME) in pts naïve to BCMA-directed therapy (Cohort A, n=123) vs. pts with prior exposure to BCMA-directed therapy (Cohort B, n=64) in MagnetisMM-3.
Methods: Pts received subcutaneous elranatamab with 2-step-up doses of 12/32 mg followed by 76 mg QW. Serum samples were collected during cycle 1, and levels of 45 cytokines were analyzed by proximity extension assay and a longitudinal mixed effects model was applied to each cytokine separately. LM22 immune cell signatures were derived from gene expression analysis of bone marrow aspirate (BMA) collected at baseline. Clinical data cutoff was January 2023 with median follow up of 12.0 months.
Results: There were no significant differences (≥2-fold; p< 0.05) in baseline levels of cytokines between BCMA-naïve and BCMA-exposed pts and no baseline cytokine correlated with the development of CRS in either group. In BCMA naïve patients, 7 cytokines (IL-6, IFN-g, IL-10, TNF-a, CCL-8, IL-27, IL-2) were differentially expressed (≥3-fold; unadjusted p< 0.05) during treatment in pts with CRS whereas in BCMA-exposed pts, only 6 cytokines (IL-10, IL-1b, IL-13, IL-18, TSL and IL-2) were differentially expressed in pts with CRS. Notably, the difference in cytokine expression in BCMA-exposed pts experiencing CRS was often smaller and/or peaked at different times than in BCMA-naïve pts, suggesting an altered cytokine response in pts with prior BCMA-directed therapy.
Patients with prior exposure to a BCMA agent were treated either with an ADC (n=46) or a CAR-T agent (n=21). At baseline, there were no significant differences (≥2-fold; p< 0.05) in cytokine levels between the ADC vs. CAR-T subgroups. In patients that experienced CRS only two cytokines were differentially expressed (≥3-fold; p< 0.05) in pts experiencing CRS: higher IL-4 in the CAR-T subgroup (3.15-fold at C1D5; p=0.002) and higher IL-1b (3.2-fold at C1D2; p=0.011 and 3.4-fold at C1D15; p=0.001) in the ADC subgroup.
Gene expression analysis of bulk BMA samples at baseline revealed a different immune cell signature with less abundant subsets of inferred T-cell populations in BCMA-exposed pts compared to BCMA naïve pts. The difference was driven by a lower abundance of T-cell population signatures in the CAR-T relative to the ADC subgroup, suggesting inherent differences in the baseline immune TME in these groups. Additionally, no significant association between CRS and baseline LM22 immune cell signatures in BCMA-naïve vs. BCMA-exposed pts was observed.
Conclusions: Cytokine induction in pts experiencing CRS in prior-exposed BCMA patients was often different compared to BCMA naïve patients. Distinct immune cell signatures derived from gene expression analysis of the TME were observed in pts with prior BCMA-directed CAR-T therapy.
Methods: Pts received subcutaneous elranatamab with 2-step-up doses of 12/32 mg followed by 76 mg QW. Serum samples were collected during cycle 1, and levels of 45 cytokines were analyzed by proximity extension assay and a longitudinal mixed effects model was applied to each cytokine separately. LM22 immune cell signatures were derived from gene expression analysis of bone marrow aspirate (BMA) collected at baseline. Clinical data cutoff was January 2023 with median follow up of 12.0 months.
Results: There were no significant differences (≥2-fold; p< 0.05) in baseline levels of cytokines between BCMA-naïve and BCMA-exposed pts and no baseline cytokine correlated with the development of CRS in either group. In BCMA naïve patients, 7 cytokines (IL-6, IFN-g, IL-10, TNF-a, CCL-8, IL-27, IL-2) were differentially expressed (≥3-fold; unadjusted p< 0.05) during treatment in pts with CRS whereas in BCMA-exposed pts, only 6 cytokines (IL-10, IL-1b, IL-13, IL-18, TSL and IL-2) were differentially expressed in pts with CRS. Notably, the difference in cytokine expression in BCMA-exposed pts experiencing CRS was often smaller and/or peaked at different times than in BCMA-naïve pts, suggesting an altered cytokine response in pts with prior BCMA-directed therapy.
Patients with prior exposure to a BCMA agent were treated either with an ADC (n=46) or a CAR-T agent (n=21). At baseline, there were no significant differences (≥2-fold; p< 0.05) in cytokine levels between the ADC vs. CAR-T subgroups. In patients that experienced CRS only two cytokines were differentially expressed (≥3-fold; p< 0.05) in pts experiencing CRS: higher IL-4 in the CAR-T subgroup (3.15-fold at C1D5; p=0.002) and higher IL-1b (3.2-fold at C1D2; p=0.011 and 3.4-fold at C1D15; p=0.001) in the ADC subgroup.
Gene expression analysis of bulk BMA samples at baseline revealed a different immune cell signature with less abundant subsets of inferred T-cell populations in BCMA-exposed pts compared to BCMA naïve pts. The difference was driven by a lower abundance of T-cell population signatures in the CAR-T relative to the ADC subgroup, suggesting inherent differences in the baseline immune TME in these groups. Additionally, no significant association between CRS and baseline LM22 immune cell signatures in BCMA-naïve vs. BCMA-exposed pts was observed.
Conclusions: Cytokine induction in pts experiencing CRS in prior-exposed BCMA patients was often different compared to BCMA naïve patients. Distinct immune cell signatures derived from gene expression analysis of the TME were observed in pts with prior BCMA-directed CAR-T therapy.
