Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-232: Effectiveness of anti-B-cell maturation antigen (BCMA)-targeting therapy after selinexor treatment
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Muhamed Baljevic, MD, FACP
Associate Professor of Medicine, Division of Hematology-Oncology
Vanderbilt-Ingram Cancer Center, Vanderbilt University Medical Center, Tennessee, United States
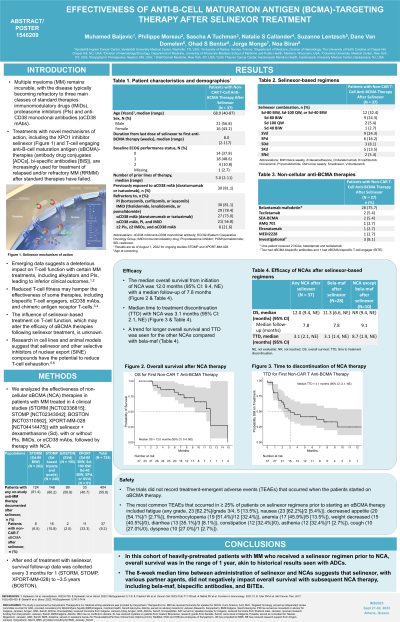
Introduction: Multiple myeloma (MM) remains incurable, with the disease typically becoming refractory to three main classes of standard therapies: immunomodulatory drugs (IMiDs), proteasome inhibitors (PIs) and anti-CD38 monoclonal antibodies (αCD38 mAbs). Treatments with novel mechanisms of action, including the XPO1 inhibitor selinexor and T-cell engaging anti-B-cell maturation antigen (αBCMA)-agents (antibody drug conjugates [ADC], bi-specific antibodies [BiS]), are increasingly used for treatment of relapsed and/or refractory MM (RRMM) after standard therapies have failed. Emerging data suggests a deleterious impact on T cell function with certain MM treatments, including alkylators and PIs, leading to inferior clinical outcomes. The influence of selinexor-based treatment on T cell function, which may alter the efficacy of αBCMA agents following selinexor treatment, is unknown.
Methods: We analyzed the effectiveness of non-cellular αBCMA (NCA) therapies in pts with MM treated in 4 clinical studies (STORM [NCT02336815]; STOMP [NCT02343042]; BOSTON [NCT03110562], XPORT-MM-028 [NCT04414475]) with selinexor + dexamethasone (Xd), with or without PIs, IMiDs, or αCD38 mAbs, followed by therapy with NCA. After end of treatment with selinexor, survival follow-up data was collected every 3 months for 1 (STORM, STOMP, XPORT-MM-028) to 5 years (BOSTON).
Results: Across the 4 clinical studies, 724 pts received selinexor, 404 of which had therapy post-selinexor documented. Thirty-seven pts (median age: 68, range: 40-87) received NCA therapy at any time following a selinexor regimen (Xd, n=12; Xd + bortezomib, n=9; Xd + pomalidomide, n=6; Xd + daratumumab, n=3; Xd + carfilzomib, n=5; Xd + ixazomib, n=2). NCAs included the ADC belantamab mafodotin (n=28), the BiS teclistamab (n=2), SEA-BCMA (n=2), AMG 701 (n=1), elranatamab (n=1), MEDI2228 (n=1), and investigational (n=3; 2 had αBCMA bispecific antibodies and 1 had αBCMA BITE) (1 pt received 2 NCAs, belantamab and teclistamab). For the selinexor-based regimens, the median number of previous lines of therapy was 5 (range: 2-11) and 21 (56.8%) pts had triple-class refractory MM including 8 (21.6%) with penta-refractory MM. Median time from last dose of selinexor to NCA was 8 weeks (range: 2-117). Median time to treatment discontinuation with NCA was 4.4 months (95% CI: 2.1, NE). The median overall survival from initiation of NCA was 12.0 months (95% CI: 9.4, NE) with a median follow-up of 7.8 months.
Conclusions: In this cohort of heavily-pretreated pts with MM who received a selinexor regimen prior to NCA, overall survival was in the range of 1 year, akin to historical results seen with ADCs. The 8-week median time between administration of selinexor and NCAs suggests that selinexor, with various partner agents, did not negatively impact overall survival with subsequent NCA therapy.
©2023 ASCO. Reused with permission. This abstract was accepted and previously presented at the 2023 ASCO Annual Meeting. All rights reserved.
Methods: We analyzed the effectiveness of non-cellular αBCMA (NCA) therapies in pts with MM treated in 4 clinical studies (STORM [NCT02336815]; STOMP [NCT02343042]; BOSTON [NCT03110562], XPORT-MM-028 [NCT04414475]) with selinexor + dexamethasone (Xd), with or without PIs, IMiDs, or αCD38 mAbs, followed by therapy with NCA. After end of treatment with selinexor, survival follow-up data was collected every 3 months for 1 (STORM, STOMP, XPORT-MM-028) to 5 years (BOSTON).
Results: Across the 4 clinical studies, 724 pts received selinexor, 404 of which had therapy post-selinexor documented. Thirty-seven pts (median age: 68, range: 40-87) received NCA therapy at any time following a selinexor regimen (Xd, n=12; Xd + bortezomib, n=9; Xd + pomalidomide, n=6; Xd + daratumumab, n=3; Xd + carfilzomib, n=5; Xd + ixazomib, n=2). NCAs included the ADC belantamab mafodotin (n=28), the BiS teclistamab (n=2), SEA-BCMA (n=2), AMG 701 (n=1), elranatamab (n=1), MEDI2228 (n=1), and investigational (n=3; 2 had αBCMA bispecific antibodies and 1 had αBCMA BITE) (1 pt received 2 NCAs, belantamab and teclistamab). For the selinexor-based regimens, the median number of previous lines of therapy was 5 (range: 2-11) and 21 (56.8%) pts had triple-class refractory MM including 8 (21.6%) with penta-refractory MM. Median time from last dose of selinexor to NCA was 8 weeks (range: 2-117). Median time to treatment discontinuation with NCA was 4.4 months (95% CI: 2.1, NE). The median overall survival from initiation of NCA was 12.0 months (95% CI: 9.4, NE) with a median follow-up of 7.8 months.
Conclusions: In this cohort of heavily-pretreated pts with MM who received a selinexor regimen prior to NCA, overall survival was in the range of 1 year, akin to historical results seen with ADCs. The 8-week median time between administration of selinexor and NCAs suggests that selinexor, with various partner agents, did not negatively impact overall survival with subsequent NCA therapy.
©2023 ASCO. Reused with permission. This abstract was accepted and previously presented at the 2023 ASCO Annual Meeting. All rights reserved.
