Treatment of Relapsed/Refractory Myeloma
Poster Session 2
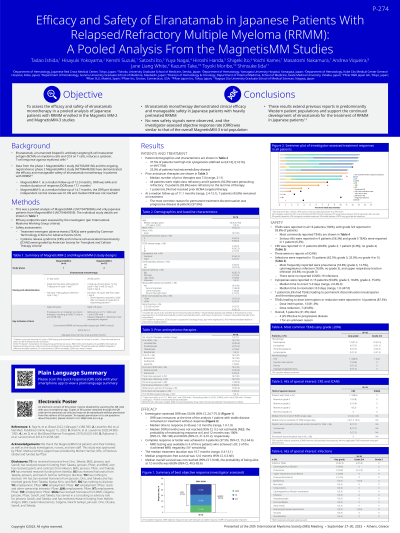
P-274: Efficacy and safety of elranatamab in Japanese patients with relapsed/refractory multiple myeloma (RRMM): A pooled analysis from the MagnetisMM studies
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST
.jpg)
Tadao Ishida, MD, PhD
Director - Hematology
Japanese Red Cross Medical Center, Tokyo, Japan, Japan
Introduction: This was a pooled analysis of Japanese patients (pts) with RRMM enrolled in the MagnetisMM studies MM-2 (NCT04798586) and MM-3 (NCT04649359) that evaluated the efficacy and safety of elranatamab.
Methods: MagnetisMM-2 was a single-arm, open-label, multicenter, phase 1 study to evaluate elranatamab monotherapy of 1000 μg/kg SC weekly, with a 600 μg/kg SC priming dose, in Japanese pts with RRMM who received ≥3 prior therapies (≥1 proteasome inhibitor (PI), ≥1 immunomodulatory drug (IMiD), and ≥1 anti-CD38 antibody). MagnetisMM-3 is an ongoing open-label, multicenter, non-randomized, phase 2 study in pts with RRMM refractory to ≥1 PI, ≥1 IMiD and ≥1 anti-CD38 antibody, with elranatamab administered SC at a fixed dose of 76 mg weekly. Pts received SC elranatamab in 28-d cycles with step-up doses of 12 mg on C1D1 and 32 mg on C1D4 followed by 76 mg QW beginning C1D8.
Results: In total, 16 pts (MM-2, n=4; MM-3, n=12) were included, 62.5% were male and median age was 68.5 y (range, 47−83). At baseline, pts had an ECOG PS of 0 (50.0%) or 1 (50.0%); 37.5% had high risk cytogenetics; 25.0% had extramedullary disease. Pts received a median of 7.0 (2−11) prior lines of therapy, all pts were triple-class refractory and 8 pts (50.0%) were penta-drug refractory, and 15 pts (93.8%) were refractory to the last line of therapy. After a median follow-up of 11.1 mo (2.4−13.1), 43.8% of pts remained on treatment; the most common reason for permanent treatment discontinuation was progressive disease (37.5%). The objective response rate by investigator was 50.0% (95% CI 24.7−75.3), although not yet mature at the time of analysis; 37.5% and 50.0% achieved complete response or better and very good partial response or better, respectively. Among responders, the median duration of response was not reached (95% CI 9.2, NE) and the probability of maintaining the response at 9 months was 100% (95% CI: 100, 100). Dose reduction or interruption due to AEs occurred in 87.5% of pts and 1 pt permanently discontinued due to AEs (neutropenia, thrombocytopenia). 15 (93.8%) of pts reported G3/4 AEs. The most common TEAEs (≥50% of pts) were neutropenia (13 (81.3%) [G3/4, 13 (81.3%)]) and CRS (11 (68.8%) [G3/4, 1 (6.3%)]). No pt had ICANS. Overall, 5 (31.3%) pts died; 4 (25%) due to disease progression, 1 (6.3%) unknown.
Conclusions: Deep and durable responses to elranatamab monotherapy were observed in Japanese pts with heavily pre-treated refractory MM. The safety profile was manageable and no new safety signals were identified. These results support the continued development of elranatamab for the treatment of RRMM in Japanese pts.
Methods: MagnetisMM-2 was a single-arm, open-label, multicenter, phase 1 study to evaluate elranatamab monotherapy of 1000 μg/kg SC weekly, with a 600 μg/kg SC priming dose, in Japanese pts with RRMM who received ≥3 prior therapies (≥1 proteasome inhibitor (PI), ≥1 immunomodulatory drug (IMiD), and ≥1 anti-CD38 antibody). MagnetisMM-3 is an ongoing open-label, multicenter, non-randomized, phase 2 study in pts with RRMM refractory to ≥1 PI, ≥1 IMiD and ≥1 anti-CD38 antibody, with elranatamab administered SC at a fixed dose of 76 mg weekly. Pts received SC elranatamab in 28-d cycles with step-up doses of 12 mg on C1D1 and 32 mg on C1D4 followed by 76 mg QW beginning C1D8.
Results: In total, 16 pts (MM-2, n=4; MM-3, n=12) were included, 62.5% were male and median age was 68.5 y (range, 47−83). At baseline, pts had an ECOG PS of 0 (50.0%) or 1 (50.0%); 37.5% had high risk cytogenetics; 25.0% had extramedullary disease. Pts received a median of 7.0 (2−11) prior lines of therapy, all pts were triple-class refractory and 8 pts (50.0%) were penta-drug refractory, and 15 pts (93.8%) were refractory to the last line of therapy. After a median follow-up of 11.1 mo (2.4−13.1), 43.8% of pts remained on treatment; the most common reason for permanent treatment discontinuation was progressive disease (37.5%). The objective response rate by investigator was 50.0% (95% CI 24.7−75.3), although not yet mature at the time of analysis; 37.5% and 50.0% achieved complete response or better and very good partial response or better, respectively. Among responders, the median duration of response was not reached (95% CI 9.2, NE) and the probability of maintaining the response at 9 months was 100% (95% CI: 100, 100). Dose reduction or interruption due to AEs occurred in 87.5% of pts and 1 pt permanently discontinued due to AEs (neutropenia, thrombocytopenia). 15 (93.8%) of pts reported G3/4 AEs. The most common TEAEs (≥50% of pts) were neutropenia (13 (81.3%) [G3/4, 13 (81.3%)]) and CRS (11 (68.8%) [G3/4, 1 (6.3%)]). No pt had ICANS. Overall, 5 (31.3%) pts died; 4 (25%) due to disease progression, 1 (6.3%) unknown.
Conclusions: Deep and durable responses to elranatamab monotherapy were observed in Japanese pts with heavily pre-treated refractory MM. The safety profile was manageable and no new safety signals were identified. These results support the continued development of elranatamab for the treatment of RRMM in Japanese pts.
