Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-255: Efficacy of a Second Autologous Stem Cell Transplant for Multiple Myeloma and Correlation with Response to Initial Transplant: A Single-Center Experience
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Barry Paul, MD, MS (he/him/his)
Assistant Professor
Atrium Health, Levine Cancer Institute
Charlotte, North Carolina, United States
Introduction: High-dose melphalan (HDM) and autologous stem cell transplant (ASCT) has consistently been shown to improve depth of response and PFS in large phase 3 trials of myeloma patients. However, the role of a second (salvage) transplant (sASCT) for relapsed refractory multiple myeloma (RRMM) in the era of novel therapies is less clear.
Methods: We retrospectively evaluated 43 RRMM patients who underwent a sASCT between Nov 2014 and June 2022 at our institution.
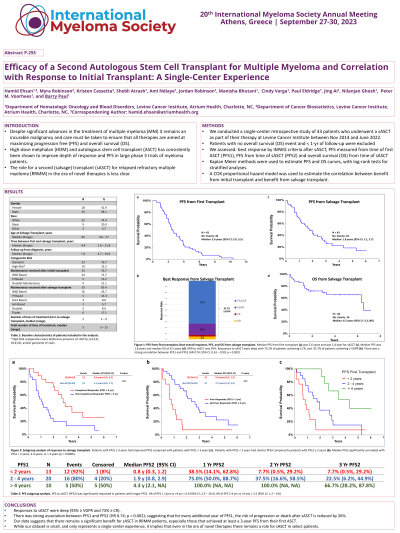
Results: Median time between first and sASCT was 4.4 yrs. The median follow-up from MM diagnosis was 7.6 yrs, and from sASCT was 2.9 yrs. The majority of pts had standard risk cytogenetics (77%). The most common cytogenetic abnormalities at diagnosis were monosomy 13 (35%) followed by t(11;14), del 17p, and gain/amp of 1q21 (each 14%). The most common induction regimen was RVD (51%) followed by CyBorD (11.6%). Most patients (76.7%) received maintenance therapy after initial transplant with IMiD (72%), PI (15%) and doublet (12.4%) regimens being most common. After sASCT the majority of patients (85.4%) received maintenance with IMiD (45%), triplet (17%), PI (14%), daratumumab (8.6%), doublets (8.6%), or Selinexor (5.7%). The median total number of lines of therapies was 5 (3-15). Two patients (4.7%) succumbed to sASCT-related mortality, with 41 patients being response-evaluable. Responses were deep, with most patients achieving a CR or sCR (70%), or VGPR (18.6%) as best response after sASCT, while only three patients (7 %) achieved < VGPR. The median PFS1 was 2.6 yrs while PSF2 was 1.8 yrs. Further, PFS1 appeared to be associated with PFS2 (HR 0.74; 95% CI: 0.61 – 0.90; p = 0.002), suggesting that for every additional year of PFS1, the risk of progression or death in subjects after sASCT is reduced by 27%. A stratified analysis looking at PFS2 in patients who had PFS1 of < 2 years (n=13), 2-4 years (n=20), or >4 years (n=10) also supported this association (log-rank test p< 0.001). Specifically, patients with PFS1 < 2 years had a median PFS2 of only 0.8 years; patients with PFS1 of 2-4 years had a median PFS2 of 2 years; while the median PFS2 for patients who had >4 years of PFS1 was 4.3 years. Using cox proportional hazards models, the risk of progression or death after sASCT in those with PFS1 < 2 years is 6.6 times compared to those with PFS1 >4 years.
Conclusions: Our data suggest a significant benefit for sASCT in RRMM patients, especially those that achieved at least a 4-year PFS from their first ASCT. Additionally, most patients achieved deep responses (CR or sCR). While our dataset is small and only represents a single-center experience, it implies that even in the era of novel therapies such as CAR-Ts and bispecific antibodies, there remains a role for sASCT in select patients.
Methods: We retrospectively evaluated 43 RRMM patients who underwent a sASCT between Nov 2014 and June 2022 at our institution.
Results: Median time between first and sASCT was 4.4 yrs. The median follow-up from MM diagnosis was 7.6 yrs, and from sASCT was 2.9 yrs. The majority of pts had standard risk cytogenetics (77%). The most common cytogenetic abnormalities at diagnosis were monosomy 13 (35%) followed by t(11;14), del 17p, and gain/amp of 1q21 (each 14%). The most common induction regimen was RVD (51%) followed by CyBorD (11.6%). Most patients (76.7%) received maintenance therapy after initial transplant with IMiD (72%), PI (15%) and doublet (12.4%) regimens being most common. After sASCT the majority of patients (85.4%) received maintenance with IMiD (45%), triplet (17%), PI (14%), daratumumab (8.6%), doublets (8.6%), or Selinexor (5.7%). The median total number of lines of therapies was 5 (3-15). Two patients (4.7%) succumbed to sASCT-related mortality, with 41 patients being response-evaluable. Responses were deep, with most patients achieving a CR or sCR (70%), or VGPR (18.6%) as best response after sASCT, while only three patients (7 %) achieved < VGPR. The median PFS1 was 2.6 yrs while PSF2 was 1.8 yrs. Further, PFS1 appeared to be associated with PFS2 (HR 0.74; 95% CI: 0.61 – 0.90; p = 0.002), suggesting that for every additional year of PFS1, the risk of progression or death in subjects after sASCT is reduced by 27%. A stratified analysis looking at PFS2 in patients who had PFS1 of < 2 years (n=13), 2-4 years (n=20), or >4 years (n=10) also supported this association (log-rank test p< 0.001). Specifically, patients with PFS1 < 2 years had a median PFS2 of only 0.8 years; patients with PFS1 of 2-4 years had a median PFS2 of 2 years; while the median PFS2 for patients who had >4 years of PFS1 was 4.3 years. Using cox proportional hazards models, the risk of progression or death after sASCT in those with PFS1 < 2 years is 6.6 times compared to those with PFS1 >4 years.
Conclusions: Our data suggest a significant benefit for sASCT in RRMM patients, especially those that achieved at least a 4-year PFS from their first ASCT. Additionally, most patients achieved deep responses (CR or sCR). While our dataset is small and only represents a single-center experience, it implies that even in the era of novel therapies such as CAR-Ts and bispecific antibodies, there remains a role for sASCT in select patients.
