Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-306: Final results of a Phase 1b study of subcutaneous isatuximab administration by an on-body delivery system (OBDS) plus pomalidomide and dexamethasone in relapsed/refractory multiple myeloma (RRMM)
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST
.jpg)
Hang Quach, MBBS(Hons) SpecCertOC FRACP FRCPA MD
Director of Haematology
St Vincent’s Hospital Melbourne, University of Melbourne, VIC, Australia
Melbourne, Victoria, Australia
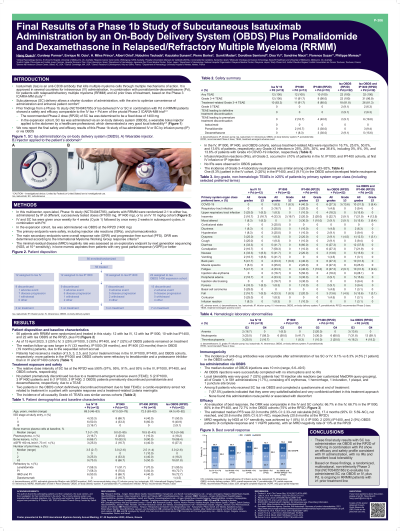
Introduction: Intravenous (IV) administration of isatuximab (Isa) plus pomalidomide-dexamethasone (Pd) is approved for patients (pts) with RRMM. Subcutaneous (SC) delivery allows a shorter duration of administration, with the aim to optimize convenience of administration and enhance patient comfort. Prior investigations in a Phase 1b study (NCT04045795) determined the recommended phase 2 dose (RP2D) for SC Isa at 1400 mg, and showed safety and efficacy for SC Isa + Pd comparable to IV Isa + Pd in the pivotal ICARIA-MM trial in RRMM pts. We now present the final safety and efficacy study results.
Methods: This multicenter Phase 1b study evaluated SC vs IV Isa + Pd in RRMM pts with ≥2 prior treatment lines including lenalidomide and a proteasome inhibitor. Pts were randomized to SC by infusion pump (IP)1000 mg or IV 10 mg/kg and to IP1400 mg or IV. In the expansion cohort, SC Isa was administered at the RP2D via OBDS, a wearable bolus injector applied to the abdomen by a healthcare professional. Safety and PK were the primary endpoints; the main secondary endpoints were overall response rate (ORR) and progression-free survival (PFS).
Results: Of the 56 randomized pts, 25% (3/12) IV, 25% (3/12) IP1000, 30% (3/10) IP1400 and 32% (7/22) of OBDS pts remained on treatment as of 15 Apr 2023. Median follow-up was 33 mo for IV, 39 mo for IP1000, 33 mo for IP1400 and 19 mo for the OBDS cohort due to the sequential accrual. ≥50% of pts had received ≥3 prior treatment lines. In the IV, IP1000, IP1400 and OBDS cohorts, serious treatment-related AEs occurred in 17%, 25%, 50% and 14% of pts; any ≥G3 infections were reported in 25%, 25%, 30% and 36% of pts including 0%, 8%, 0% and 14% ≥G3 Covid-19, respectively. Median duration of OBDS injections was 10 min (6.6-49.5); all injections were completed successfully with no interruption and no infusion reactions (IRs). Local tolerability was good: 7 (32%) pts had 10 injection site reactions, all G1, in 581 administrations (1.7%), mainly erythemas. The relative dose intensity of Isa at the SC RP2D was ≥90% (97%, 95%, 91% and 93% in the IV, IP1000, IP1400 and OBDS cohorts, respectively). ORR was 66.7% in the IV, 66.7% in the IP1000, 80% in the IP1400, and 72.7% in the OBDS cohorts (75% at the RP2D). Median PFS was 22.0 mo, 17.4 mo, not reached and 20.6 mo, respectively (20.6 mo at the RP2D). Minimal residual disease negativity (by NGS) at 10-5 sensitivity was achieved by 1/12 (8%) IV, 0/12 IP1000, 2/10 (20%) IP1400 and 2/22 (9%) OBDS pts (4 CR, 1 VGPR pts) (13% at the RP2D). The incidence of anti-drug antibodies appeared comparable after administration of Isa SC or IV (9.1% vs 8.3%).
Conclusions: Final study results with SC Isa administration via OBDS at the 1400 mg RP2D + Pd show an efficacy and safety profile consistent with IV administration, with no IRs, and excellent local tolerability. A non-inferiority Phase 3 trial (NCT05405166) evaluating SC Isa via OBDS versus IV Isa is ongoing.
Methods: This multicenter Phase 1b study evaluated SC vs IV Isa + Pd in RRMM pts with ≥2 prior treatment lines including lenalidomide and a proteasome inhibitor. Pts were randomized to SC by infusion pump (IP)1000 mg or IV 10 mg/kg and to IP1400 mg or IV. In the expansion cohort, SC Isa was administered at the RP2D via OBDS, a wearable bolus injector applied to the abdomen by a healthcare professional. Safety and PK were the primary endpoints; the main secondary endpoints were overall response rate (ORR) and progression-free survival (PFS).
Results: Of the 56 randomized pts, 25% (3/12) IV, 25% (3/12) IP1000, 30% (3/10) IP1400 and 32% (7/22) of OBDS pts remained on treatment as of 15 Apr 2023. Median follow-up was 33 mo for IV, 39 mo for IP1000, 33 mo for IP1400 and 19 mo for the OBDS cohort due to the sequential accrual. ≥50% of pts had received ≥3 prior treatment lines. In the IV, IP1000, IP1400 and OBDS cohorts, serious treatment-related AEs occurred in 17%, 25%, 50% and 14% of pts; any ≥G3 infections were reported in 25%, 25%, 30% and 36% of pts including 0%, 8%, 0% and 14% ≥G3 Covid-19, respectively. Median duration of OBDS injections was 10 min (6.6-49.5); all injections were completed successfully with no interruption and no infusion reactions (IRs). Local tolerability was good: 7 (32%) pts had 10 injection site reactions, all G1, in 581 administrations (1.7%), mainly erythemas. The relative dose intensity of Isa at the SC RP2D was ≥90% (97%, 95%, 91% and 93% in the IV, IP1000, IP1400 and OBDS cohorts, respectively). ORR was 66.7% in the IV, 66.7% in the IP1000, 80% in the IP1400, and 72.7% in the OBDS cohorts (75% at the RP2D). Median PFS was 22.0 mo, 17.4 mo, not reached and 20.6 mo, respectively (20.6 mo at the RP2D). Minimal residual disease negativity (by NGS) at 10-5 sensitivity was achieved by 1/12 (8%) IV, 0/12 IP1000, 2/10 (20%) IP1400 and 2/22 (9%) OBDS pts (4 CR, 1 VGPR pts) (13% at the RP2D). The incidence of anti-drug antibodies appeared comparable after administration of Isa SC or IV (9.1% vs 8.3%).
Conclusions: Final study results with SC Isa administration via OBDS at the 1400 mg RP2D + Pd show an efficacy and safety profile consistent with IV administration, with no IRs, and excellent local tolerability. A non-inferiority Phase 3 trial (NCT05405166) evaluating SC Isa via OBDS versus IV Isa is ongoing.
