Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-276: Healthcare Resource Utilization and Costs Among Patients With Relapsed/Refractory Multiple Myeloma Treated With Chimeric Antigen Receptor-T (CAR-T) Cell Therapy
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Sundar Jagannath, MD, FASCO
Chair for Multiple Myeloma and Professor of Medicine
Mount Sinai Medical Center, New York, NY, USA
New York, New York, United States
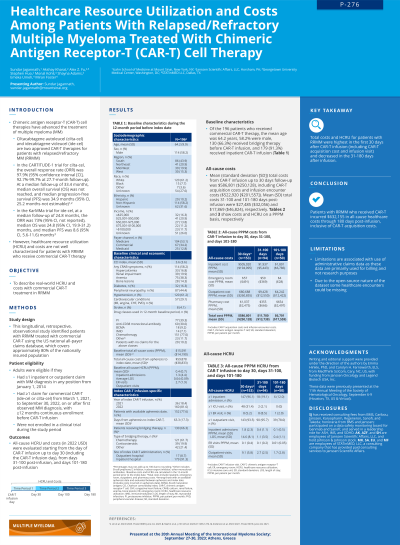
Introduction: Chimeric antigen receptor-T (CAR-T) therapies have advanced treatment of multiple myeloma (MM); however, healthcare resource utilization (HCRU) and costs are not well characterized for patients with relapsed/refractory MM (RRMM) who receive commercial CAR-T therapy. The study aim was to describe real-world HCRU and costs in patients with RRMM who received commercial CAR-T treatment.
Methods: This longitudinal, retrospective, observational study identified patients with RRMM treated with commercial CAR-T using the US national all-payer claims database that covers approximately 80% of the nationally insured population. Adults were eligible if they had ≥1 inpatient or outpatient claim with MM diagnosis and ≥1 claim for commercial CAR-T (idecabtagene vicleucel or ciltacabtagene autoleucel) from March 1, 2021, to September 30, 2022, with ≥12 months continuous enrollment before CAR-T infusion and if they were not enrolled in a clinical trial during the study period. All-cause HCRU and costs (in 2022 US $) were evaluated starting from the day of CAR-T infusion up to day 30 and from day 31 to 100 and day 101 to 180 post-infusion.
Results: Of the 196 patients who received commercial CAR-T therapy, the mean age was 64.2 years, 58.2% were male, 130 (66.3%) received bridging therapy before CAR-T infusion, and 179 (91.3%) received inpatient CAR-T infusion. Including the day of CAR-T infusion up to 30-day follow-up (n=153), mean (standard deviation [SD]) total all-cause cost per patient per month (PPPM) was $586,801 ($250,128) inclusive of CAR-T drug costs and infusion encounter costs (mean [SD], $522,920 [$201,557]). Mean (SD) total cost PPPM from day 31 to 100 (n=94) and day 101 to 180 (n=50) post-infusion was $11,780 ($13,738) and $6,701 ($17,559), respectively. Including CAR-T infusion day to 30-day follow-up, mean (SD) number of inpatient admissions was 1.8 (2.3) PPPM with a mean (SD) length of stay (LOS) of 14.6 (8.1) days PPPM; 5.2% had ≥1 emergency room (ER) visit; and mean (SD) number of outpatient visits PPPM was 9.1 (5.8). From 31 to 100 days post-infusion, mean (SD) number of outpatient visits PPPM was 2.7 (2.5); 8.5% had ≥1 ER visit; and mean (SD) inpatient admissions PPPM was 0.4 (1.1) with a mean (SD) LOS of 1.1 (3.5) days PPPM. From 101 to 180 days post-infusion, mean (SD) number of outpatient visits PPPM was 1.7 (2.8); 2.0% had ≥1 ER visit; and mean (SD) number of inpatient admissions PPPM was 0.1 (0.5) with a mean (SD) LOS of 0.4 (1.1) days PPPM.
Conclusions: Patients with RRMM who received CAR-T incurred ~$632,000 in all-cause healthcare costs through 180 days post-infusion, inclusive of CAR-T drug costs. HCRU and costs tapered beyond 30 days to 180 days post-infusion.
Methods: This longitudinal, retrospective, observational study identified patients with RRMM treated with commercial CAR-T using the US national all-payer claims database that covers approximately 80% of the nationally insured population. Adults were eligible if they had ≥1 inpatient or outpatient claim with MM diagnosis and ≥1 claim for commercial CAR-T (idecabtagene vicleucel or ciltacabtagene autoleucel) from March 1, 2021, to September 30, 2022, with ≥12 months continuous enrollment before CAR-T infusion and if they were not enrolled in a clinical trial during the study period. All-cause HCRU and costs (in 2022 US $) were evaluated starting from the day of CAR-T infusion up to day 30 and from day 31 to 100 and day 101 to 180 post-infusion.
Results: Of the 196 patients who received commercial CAR-T therapy, the mean age was 64.2 years, 58.2% were male, 130 (66.3%) received bridging therapy before CAR-T infusion, and 179 (91.3%) received inpatient CAR-T infusion. Including the day of CAR-T infusion up to 30-day follow-up (n=153), mean (standard deviation [SD]) total all-cause cost per patient per month (PPPM) was $586,801 ($250,128) inclusive of CAR-T drug costs and infusion encounter costs (mean [SD], $522,920 [$201,557]). Mean (SD) total cost PPPM from day 31 to 100 (n=94) and day 101 to 180 (n=50) post-infusion was $11,780 ($13,738) and $6,701 ($17,559), respectively. Including CAR-T infusion day to 30-day follow-up, mean (SD) number of inpatient admissions was 1.8 (2.3) PPPM with a mean (SD) length of stay (LOS) of 14.6 (8.1) days PPPM; 5.2% had ≥1 emergency room (ER) visit; and mean (SD) number of outpatient visits PPPM was 9.1 (5.8). From 31 to 100 days post-infusion, mean (SD) number of outpatient visits PPPM was 2.7 (2.5); 8.5% had ≥1 ER visit; and mean (SD) inpatient admissions PPPM was 0.4 (1.1) with a mean (SD) LOS of 1.1 (3.5) days PPPM. From 101 to 180 days post-infusion, mean (SD) number of outpatient visits PPPM was 1.7 (2.8); 2.0% had ≥1 ER visit; and mean (SD) number of inpatient admissions PPPM was 0.1 (0.5) with a mean (SD) LOS of 0.4 (1.1) days PPPM.
Conclusions: Patients with RRMM who received CAR-T incurred ~$632,000 in all-cause healthcare costs through 180 days post-infusion, inclusive of CAR-T drug costs. HCRU and costs tapered beyond 30 days to 180 days post-infusion.
