Myeloma Genomics and cell signaling
Poster Session 3
P-367: High-risk cytogenetic abnormalities in Multiple Myeloma: PETHEMA-GEM experience.
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST
.jpg)
Paula Rodríguez-Otero, MD, PhD (she/her/hers)
Associate Professor
Clínica Universidad de Navarra, CIMA, CIBERONC, IDISNA, Pamplona, Spain
Pamplona, Navarra, Spain
Introduction: Multiple myeloma (MM) is a diverse disease both clinically and genetically. This study aims to analyze the impact of cytogenetic abnormalities detected through fluorescence in situ hybridization (FISH) and the role of co-segregation on prognosis in newly diagnosed MM patients.
Methods: We have investigated the presence of t(4;14), t(14;16), 17p deletion, +1q (gain/amplification) and 1p deletion by FISH on CD38 purified plasma cells. The cut-off level for considering a positive result was set at 10% for IGH translocations (fusion/break-apart probes), and 20% for gains and deletions. For +1q, gain was defined as 3 copies (1q gain), and 1q amplification as ≥4 copies (amp1q). Statistical analyses were performed to compare different groups and evaluate progression-free survival (PFS) and overall survival (OS). The Cox proportional hazards regression model was employed to estimate hazard ratios and 95% confidence intervals.
Results: A total of 1304 patients enrolled in 4 trials (GEM05MAS65, GEM05MENOS65, GEM2010, and GEM2012) were included in the study. The frequencies of genetic abnormalities were: del(17p) in 8%, t(4;14) in 12%, t(14;16) in 3%, +1q in 43%, and del(1p) in 8%. The median follow-up was 61 months. The median PFS was 44 months, and the median OS was not yet reached.
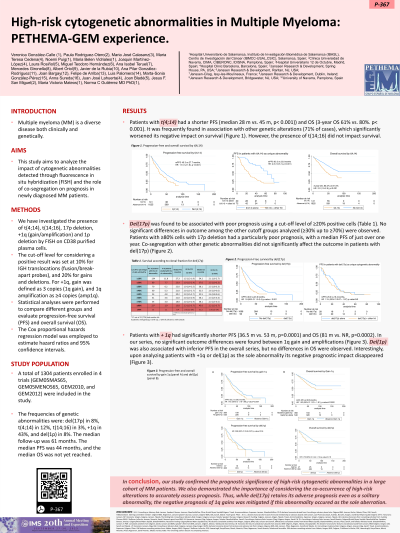
Patients with t(4;14) had a shorter PFS (median 28 m vs. 45 m, p< 0.001)) and OS (3-year OS 61% vs. 80%. p< 0.001). It was frequently found in association with other genetic alterations (71% of cases), which significantly worsened its negative impact on survival. However, the presence of t(14;16) did not impact survival.
Del(17p) was found to be associated with poor prognosis using a cut-off level of ≥20% positive cells. No significant differences in outcome among the other cutoff groups analyzed (≥30% up to ≥70%) were observed. Patients with ≥80% cells with 17p deletion had a particularly poor prognosis, with a median PFS of just over one year. Co-segregation with other genetic abnormalities did not significantly affect the outcome in patients with del(17p).
Patients with + 1q had significantly shorter PFS (36.5 m vs. 53 m, p=0.0001) and OS (81 m vs. NR, p=0.0002). In our series, no significant outcome differences were found between 1q gain and amplifications. Del(1p) was also associated with inferior PFS in the overall series, but no differences in OS were observed. Interestingly, upon analyzing patients with +1q ordel( 1p) as the sole abnormality its negative prognostic impact disappeared.
Conclusions: In conclusion, our study confirmed the prognostic significance of high-risk cytogenetic abnormalities in a large cohort of MM patients. We also demonstrated the importance of considering the co-occurrence of high-risk alterations to accurately assess prognosis. Thus, while del(17p) retains its adverse prognosis even as a solitary abnormality, the negative prognosis of 1q gains was mitigated if this abnormality occured as the sole aberration.
Methods: We have investigated the presence of t(4;14), t(14;16), 17p deletion, +1q (gain/amplification) and 1p deletion by FISH on CD38 purified plasma cells. The cut-off level for considering a positive result was set at 10% for IGH translocations (fusion/break-apart probes), and 20% for gains and deletions. For +1q, gain was defined as 3 copies (1q gain), and 1q amplification as ≥4 copies (amp1q). Statistical analyses were performed to compare different groups and evaluate progression-free survival (PFS) and overall survival (OS). The Cox proportional hazards regression model was employed to estimate hazard ratios and 95% confidence intervals.
Results: A total of 1304 patients enrolled in 4 trials (GEM05MAS65, GEM05MENOS65, GEM2010, and GEM2012) were included in the study. The frequencies of genetic abnormalities were: del(17p) in 8%, t(4;14) in 12%, t(14;16) in 3%, +1q in 43%, and del(1p) in 8%. The median follow-up was 61 months. The median PFS was 44 months, and the median OS was not yet reached.
Patients with t(4;14) had a shorter PFS (median 28 m vs. 45 m, p< 0.001)) and OS (3-year OS 61% vs. 80%. p< 0.001). It was frequently found in association with other genetic alterations (71% of cases), which significantly worsened its negative impact on survival. However, the presence of t(14;16) did not impact survival.
Del(17p) was found to be associated with poor prognosis using a cut-off level of ≥20% positive cells. No significant differences in outcome among the other cutoff groups analyzed (≥30% up to ≥70%) were observed. Patients with ≥80% cells with 17p deletion had a particularly poor prognosis, with a median PFS of just over one year. Co-segregation with other genetic abnormalities did not significantly affect the outcome in patients with del(17p).
Patients with + 1q had significantly shorter PFS (36.5 m vs. 53 m, p=0.0001) and OS (81 m vs. NR, p=0.0002). In our series, no significant outcome differences were found between 1q gain and amplifications. Del(1p) was also associated with inferior PFS in the overall series, but no differences in OS were observed. Interestingly, upon analyzing patients with +1q ordel( 1p) as the sole abnormality its negative prognostic impact disappeared.
Conclusions: In conclusion, our study confirmed the prognostic significance of high-risk cytogenetic abnormalities in a large cohort of MM patients. We also demonstrated the importance of considering the co-occurrence of high-risk alterations to accurately assess prognosis. Thus, while del(17p) retains its adverse prognosis even as a solitary abnormality, the negative prognosis of 1q gains was mitigated if this abnormality occured as the sole aberration.
